America's Vaccination Problem
Politics Trump Public Health
The United States is confronting a serious resurgence of vaccine-preventable diseases, exemplified by the measles outbreak in Texas and New Mexico that has now infected over 124 people and claimed the life of an unvaccinated child. This crisis coincides with multiple failures in public health leadership and unprecedented political interference in evidence-based practice.
Recent Centers for Disease Control and Prevention (CDC) analysis reveals that the percentage of children with a vaccine-hesitant parent varies dramatically by vaccine type — from 56% for COVID-19 vaccines to 12% for routine childhood vaccines. This growing hesitancy has created dangerous gaps in community protection across the country.
In a rapid succession of alarming developments within a single week, we've witnessed a new confirmed measles case in Kentucky from an international traveler, Health and Human Services (HHS) Secretary Robert F. Kennedy (RFK) Jr.'s cancellation of a multimillion-dollar project to develop an oral COVID-19 vaccine, and the FDA's abrupt cancellation of a critical advisory committee meeting on next season's flu vaccine formulation. During his first cabinet meeting appearance, Kennedy incorrectly stated there had been two measles deaths (there was one) and downplayed the outbreak as "not unusual" — a claim physicians immediately contradicted.
This confluence of declining vaccination rates, active disease outbreaks, and systematic dismantling of public health infrastructure represents a crisis entirely of our own making. It’s 2025 and children are dying from diseases we've known how to prevent for decades, not because of scientific limitations, but because of a collective failure to prioritize evidence over ideology.
A Dismantling in Real Time
At the February 27 cabinet meeting, HHS Secretary Kennedy made several troubling statements about the ongoing measles outbreak. "Measles outbreaks are not unusual," Kennedy claimed, an assertion quickly refuted by medical experts.
"Classifying it as 'not unusual' would be inaccurate," said Dr. Christina Johns, a pediatric emergency physician. "Usually an outbreak is in the order of a handful, not over 100 people that we have seen recently with this latest outbreak in West Texas."
Dr. Philip Huang, director of Dallas County Health and Human Services, was more direct: "This is not usual. Fortunately, it's not usual, and it's been because of the effectiveness of the vaccine."
Kennedy's statement that two people had died from measles was also incorrect – Texas officials confirmed there has been one death, an unvaccinated school-aged child. His claim that patients were hospitalized "mainly for quarantine" was astonishingly false. Local health officials reported that most patients required treatment for serious respiratory issues, including supplemental oxygen and IV fluids.
Meanwhile, in just his first two weeks in office, Kennedy has taken several actions that threaten to undermine vaccine development and public health guidance:
The FDA's Vaccines and Related Biological Products Advisory Committee (VRBPAC) meeting scheduled for March was abruptly canceled. This annual meeting is crucial for selecting the strains to be included in next season's flu vaccines. A wise move in the middle of the worst flu season in 15 years. Norman Baylor, former director of the FDA's Office of Vaccine Research and Review, told NBC News: "I'm quite shocked. The VRBPAC is critical for making the decision on strain selection for the next influenza vaccine season."
Kennedy halted a $460 million contract with Vaxart to develop a new COVID-19 vaccine in pill form, just days before 10,000 people were scheduled to begin clinical trials.
Just days earlier, Kennedy indefinitely postponed a meeting of the CDC's Advisory Committee on Immunization Practices (ACIP), which helps determine vaccine recommendations for states and insurers.
Dr. Paul Offit, a member of VRBPAC and vaccine expert at Children's Hospital of Philadelphia, expressed his dismay: "I feel like the world is upside down. We aren't doing the things we need to do to protect ourselves."
Evidence of Vaccine Success Amid Political Attacks
In striking irony, the CDC Morbidity and Mortality Weekly Report (MMWR) just published new data demonstrating the remarkable success of the human papillomavirus (HPV) vaccination program in preventing cervical cancer. During 2008–2022, cervical precancer incidence decreased 79% among screened women aged 20–24 years, the age group most likely to have been vaccinated. Higher-grade precancer incidence decreased 80% in the same group.
This success story illustrates what effective vaccination programs can achieve when supported by consistent policy and healthcare provider recommendations. The HPV vaccine has prevented countless future cancers in a generation of young people, with similar potential for other vaccines when politics doesn't interfere with public health.
The contrast between this evidence of vaccine success and the current administration's assault on public health infrastructure could not be more glaring. At the very moment when scientific data confirms vaccines' life-saving impact, political appointees are systematically dismantling the systems designed to implement and monitor vaccination programs.
The False Promise of "Informed Consent"
Kennedy has justified halting vaccine promotion by claiming he wants future campaigns to focus on "informed consent" instead. However, experts warn this framing misrepresents the concept and creates dangerous misperceptions about vaccines (which, to be fair, would make it right in RFK Jr.’s wheelhouse—if only that were the actual job description).
Mark Navin, Lainie Friedman Ross, and Jason A. Wasserman explained in STAT News: "True 'informed consent' requires an understanding of how people process information about risks, and public health must promote collective benefits rather than focus entirely on individual autonomy."
Simply listing potential vaccine side effects without context creates predictable cognitive biases, similar to hearing about a shark attack and becoming afraid to swim despite the infinitesimal risk. As these experts note, "It is more like handing someone a list of everything that could go wrong on an airplane without mentioning that flying is far safer than driving."
The CDC's canceled 'Wild to Mild' campaign appropriately conveyed what matters most: vaccines' ability to turn severe, potentially deadly disease cases into manageable, mild illnesses—reducing hospitalizations, complications, and deaths. Replacing this messaging with uncontextualized risk information isn't enhancing informed consent — it's promoting fear and hesitancy.
The Expanding Measles Threat
Measles is making a dangerous comeback. The Kentucky Department of Health confirmed its first case since 2023 in an adult who recently traveled internationally. While contagious, the individual visited a Planet Fitness gym, potentially exposing others—a not-so-subtle reminder that wiping down equipment is more than just good manners.
This case adds to outbreaks in nine states, including Texas, New Mexico, Alaska, Georgia, New Jersey, New York, and Rhode Island. The most severe remains in West Texas’ Gaines County, where nearly 14% of schoolchildren have religious exemptions from required vaccinations.
On February 26, an unvaccinated child in that Texas community became the first U.S. measles fatality since 2015 and the first pediatric death since 2003. Before vaccines, measles killed 400 to 500 Americans annually.
These outbreaks are particularly tragic given that the MMR vaccine is exceptionally safe and effective. Two doses provide 97% protection against a disease that, without vaccination, would infect nearly every child by age 15. Among 10,000 measles cases, 10 to 30 children will die, 2,000 will require hospitalization, and over 1,500 will suffer serious complications, some with lifelong consequences.
By contrast, severe vaccine side effects are extraordinarily rare—fewer than four in 10,000 people experience fever-related seizures, blood clotting issues, or allergic reactions. As beloved children’s author Roald Dahl wrote after losing his daughter Olivia to measles encephalitis in 1962: "I think it is almost a crime to allow your child to go unimmunized."
Roald Dahl and the open letter he wrote in 1986, encouraging parents to vaccinate their children against measles. (Credit: Ronald Dumont/Daily Express/Getty Images)
Declining Vaccination Rates
Vaccination rates for measles and other preventable diseases have been trending downward, creating dangerous gaps in community protection. According to research from the Center for American Progress, kindergarten MMR vaccination rates have fallen below the critical 95% threshold needed for herd immunity. Since the 2019-20 school year, coverage has dropped from 95% to approximately 93% nationwide, leaving over 250,000 children vulnerable to infection.
This decline is even more concerning at the state level. Thirty-nine states saw vaccination rates fall below the 95% threshold in the 2023-24 school year, an increase from 28 states during the 2019-20 school year. Overall, less than 93% of kindergarten children were up to date on their state-required vaccines in 2023-24, compared with 95% four years earlier.
COVID-19 and influenza vaccination rates show similar concerning trends. According to the CDC's vaccination tracking data, only 23.1% of adults have received the 2024-25 COVID vaccine, while 45.3% have received the seasonal flu vaccine. For adults 65 and older, these rates are somewhat higher but still insufficient – 44.4% for COVID and 70.2% for flu.
A 2022 modeling study estimated that over 9.1 million children (13.1%) in the United States are currently susceptible to measles infection. If pandemic-level vaccination declines persist without catch-up efforts, that number could rise to over 15 million children (21.7%), significantly increasing the risk of larger and more frequent outbreaks.
When Vaccines Become Political Identifiers
Vaccine-preventable diseases disproportionately impact vulnerable communities. Flu vaccination rates vary significantly by race, with 49% of White adults vaccinated, compared to 42% of Black adults and 35% of Hispanic adults. These disparities stem from access barriers, medical mistrust, and inconsistent provider recommendations.
The politicization of vaccines exacerbates these challenges. Support for school vaccine mandates has dropped from 82% in 2019 to 70% in 2023, driven by a sharp decline among Republicans (79% to 57%), while Democratic support remains stable at 85-88%. Similar trends appear among White evangelical Protestants, where support for school vaccine requirements fell from 77% to 58%. This geographic clustering of under-vaccinated populations fuels outbreaks—exactly what’s unfolding in West Texas.
Partisan divides extend beyond COVID-19. Republicans report lower annual flu vaccination rates than Democrats (41% vs. 56%), and among those fully vaccinated against COVID-19, Democrats are nearly three times as likely to have received a recent booster (32% vs. 12%). Vaccine hesitancy also correlates with education levels, further compounding risks in communities with both lower socioeconomic status and conservative political leanings.
Addressing these disparities requires public health strategies that acknowledge political polarization while working beyond it. Culturally tailored messaging, trusted community voices, and policies that eliminate access barriers are essential to counteract the social and ideological forces shaping vaccine decisions today.
State-Level Assaults: Louisiana's Ban on Vaccine Promotion
Federal attacks on vaccine policy are now playing out at the state level. In February 2025, the Louisiana Department of Health announced it would no longer promote mass vaccination through health fairs or media campaigns—a directive from Surgeon General Dr. Ralph Abraham that drew immediate backlash from the medical community.
Nine state medical organizations, including the Louisiana State Medical Society, issued a joint letter condemning the move: "Immunizations should not be politicized. Healthcare should not be politicized. Public health should not be politicized. Your relationship with your physician should not be politicized."
Dr. Vincent Shaw, president of the Louisiana Academy of Family Physicians, called the opposition unprecedented and warned that halting vaccine promotion could bring back diseases he's "only seen in textbooks, like measles and rubella." Meanwhile, Abraham has misrepresented his credentials, falsely identifying as a board-certified family medicine physician—raising serious concerns about the expertise guiding public health policy.
The consequences are already surfacing. Dr. Mikki Bouquet, a Baton Rouge pediatrician, reports growing parental skepticism about routine vaccinations. "Now parents are asking which vaccines are really necessary. That's absurd—it’s like asking which vitamin matters most. You need them all."
Even Republican Senator Bill Cassidy, despite voting to confirm RFK Jr. as HHS Secretary, has criticized the policy, warning that cutting vaccine outreach ignores the reality of parents' lives.
This shift underscores a troubling trend: political ideology overriding evidence-based public health, with the most vulnerable populations poised to suffer the consequences.
The Fight for Evidence-Based Solutions
This past week has marked a dangerous escalation of political interference in public health. The cancellation of vaccine advisory meetings, the halting of innovative vaccine development, and the downplaying of a deadly measles outbreak signal a fundamental shift away from science-based policy.
Healthcare professionals can no longer afford to stay on the sidelines. Beyond their clinical roles, they must become active policy advocates by:
Contacting state and federal representatives to oppose policies that undermine vaccination
Engaging with professional organizations to develop unified advocacy efforts
Providing expert testimony at legislative hearings on vaccine-related bills
Writing op-eds and speaking to media about vaccine safety and efficacy
Countering misinformation as trusted community voices
Supporting candidates who prioritize evidence-based public health policies
Medical organizations must also wield their influence more effectively. The recent joint statement from nine Louisiana medical groups demonstrates the power of unified action, while hospital systems—often major employers—hold political capital that should be used to safeguard public health infrastructure.
Community advocates play a critical role, too. Parents, faith leaders, and business owners can amplify vaccine messaging and reinforce public health norms. Even conservatives who support science-based medicine must speak out. As Senator Bill Cassidy’s rebuke of Louisiana’s vaccine policy shows, principled advocacy can transcend partisan divides when children's health is at stake.
The choice is clear: we either defend decades of vaccination progress or risk a return to the preventable suffering of the pre-vaccine era. Healthcare providers willing to advocate beyond clinic walls will determine which path we take.
DoxyPEP's Impact: New Evidence Shows Promise and Challenges in STI Prevention
After nearly two decades of rising sexually transmitted infection (STI) rates in the United States, the Centers for Disease Control & Prevention (CDC) 2023 surveillance report reveals a welcome shift: overall STI rates dropped by 1.8% from 2022 to 2023. Gonorrhea cases declined by 7% for the second straight year, and primary and secondary syphilis fell by 10%—marking the first significant decrease in more than two decades. While these figures offer cautious optimism, questions remain about how best to sustain momentum, especially amid ongoing concerns about antimicrobial resistance and unequal access to prevention resources.
One potentially transformative intervention gaining traction is doxycycline post-exposure prophylaxis (doxyPEP). The CDC’s 2024 guidelines recommend doxyPEP for gay, bisexual, and other men who have sex with men (MSM), as well as transgender women, who have experienced a bacterial STI in the past year. Although clinical trials showed promising efficacy against chlamydia and syphilis, real-world data underscore nuanced challenges related to resistance, health disparities, and local healthcare capacity.
The Changing Landscape of STI Prevention
Several initiatives set the stage for the recent slowdown in STI rates. The American Rescue Plan Act of 2021 provided funding to strengthen the disease intervention specialist workforce, bolstering capacity for targeted contact tracing and clinical follow-up. These efforts were amplified by new CDC recommendations that formalized doxyPEP for specific high-risk groups.
San Francisco became an early adopter of doxyPEP guidelines in October 2022, leveraging its established HIV prevention infrastructure and community partnerships. Early clinical trial data had shown marked drops in chlamydia and syphilis, prompting local officials to adopt prophylactic antibiotic use despite concerns over potential misuse and growing gonococcal resistance. Their experience would soon be mirrored and examined in other healthcare settings.
Real-World Evidence: San Francisco and Kaiser Permanente
Two new studies illuminate the impact of doxyPEP beyond controlled clinical environments. The first, conducted by the San Francisco Department of Public Health, examined STI rates before and after the city’s 2022 adoption of doxyPEP guidelines. Investigators reported a 49.6% drop in chlamydia and a 51.4% decline in early syphilis compared to what forecasts had predicted. Three sentinel STI clinics observed that 19.5% of eligible gay, bisexual, and other men who have sex with men, as well as transgender women, initiated doxyPEP—a relatively high uptake for a new intervention.
A complementary Kaiser Permanente Northern California study included more than 11,000 participants already on HIV pre-exposure prophylaxis (PrEP). Those who added doxyPEP to their prevention repertoire saw chlamydia rates fall from 9.6% to 2.0% every quarter, while syphilis rates declined from 1.7% to 0.3%. These improvements closely mirrored prior clinical trial data, underscoring doxyPEP’s real-world effectiveness in high-risk populations.
However, the two studies diverged in their findings on gonorrhea. San Francisco observed a 25.6% increase in gonorrhea cases among the doxyPEP group, while Kaiser Permanente achieved a modest 12% reduction. Even in the latter setting, the intervention had varying efficacy based on infection site, with minimal impact on pharyngeal gonorrhea. Researchers attribute these discrepancies to existing tetracycline resistance patterns, which can range from 20% in U.S. gonorrhea strains to over 50% in certain regions globally.
Key Challenges to Implementation
1. Antimicrobial Resistance
Chief among concerns is the capacity of gonorrhea and other pathogens to develop resistance to tetracyclines. A modeling study in The Lancet warns that if doxyPEP achieves very high uptake—around 90%—it could lose effectiveness within just 1.6 years. More moderate adoption might prolong utility but still faces the ever-present risk that gonococcal strains could quickly evolve. The tension between scaling up prophylaxis to curb infections and preserving antibiotic utility for the long term remains a core dilemma for public health agencies.
2. Limited Healthcare Infrastructure
Successfully rolling out doxyPEP also requires robust clinical infrastructures. San Francisco’s early adoption relied on specialized STI clinics, disease intervention specialists, and strong community engagement. Such resources are scarce in many rural areas and underresourced urban centers, where STI burdens are often high. Without targeted funding and workforce development, these regions may fail to realize the potential benefits of prophylaxis. This gap underscores why a one-size-fits-all strategy for doxyPEP is unlikely to work uniformly nationwide.
3. Cost and Insurance Access
The Kaiser Permanente experience highlighted how commercial insurance coverage can determine doxyPEP uptake. Though Kaiser found no racial or ethnic disparities in its cohort, the ability to pay for routine tests and antibiotics remains a significant hurdle for many. Nearly half of all new STIs affect patients aged 15–24, a demographic often lacking stable insurance. Safety-net providers, such as community clinics and public health agencies, will need additional resources to prevent cost barriers from fueling inequities in STI prevention.
Addressing Health Equity
Disparities in STI burden persist despite national declines. CDC data show that Black communities—though comprising just 12.6% of the population—face roughly a third of all reported STIs, and American Indian and Alaska Native populations have the highest rates of syphilis. These patterns reflect structural inequities, from healthcare access to economic stability. DoxyPEP, if expanded, could either narrow or widen these gaps, depending on implementation strategies.
For example, the San Francisco Department of Public Health’s success relied on partnerships with community-based organizations that serve LGBTQ+ populations, bilingual outreach, and peer educators who could directly address stigma. Similar culturally tailored approaches will be crucial elsewhere. Nationally, any prophylaxis effort must acknowledge social determinants of health, from limited insurance coverage to historical medical mistrust, as central issues in achieving equitable outcomes.
Policy Recommendations
Meeting these challenges head-on requires collaboration among federal agencies, healthcare systems, and local organizations. Four policy domains stand out:
Robust Surveillance and Resistance Tracking
Establish or enhance regional testing to promptly detect shifts in gonococcal resistance.
Standardize reporting on doxyPEP uptake, stratifying data by race, ethnicity, and insurance status to monitor equity.
Integrated Healthcare Delivery
Incorporate doxyPEP into existing HIV PrEP programs, leveraging shared clinical workflows for ongoing STI screening.
Provide decision-support tools to guide providers in identifying those most likely to benefit from prophylaxis and in understanding local resistance rates.
Financing and Insurance Coverage
Secure coverage mandates or subsidies so that the costs of antibiotics and regular STI tests do not fall disproportionately on those most at risk.
Offer grants or incentives for safety-net clinics to scale up prevention services, including patient education and follow-up testing.
Antimicrobial Stewardship and Patient Education
Develop guidelines for targeted doxyPEP use to minimize unnecessary exposure—especially for gonorrhea, given its evolving resistance.
Emphasize correct usage and follow-up testing in patient education to ensure prophylaxis remains effective and that potential side effects are promptly reported.
Looking Ahead: Balancing Innovation and Stewardship
DoxyPEP’s success in specific cohorts highlights how targeted prophylaxis can substantially reduce chlamydia and syphilis infections. However, higher gonococcal resistance in some locales points to the need for continual surveillance and swift policy adjustments. Achieving a balance between curbing acute STI outbreaks and safeguarding long-term antibiotic effectiveness will require:
Adaptive Guidelines: Quickly revising prescribing recommendations if local data reveal resistance spikes.
Equitable Implementation: Ensuring consistent uptake in historically underserved communities, rather than concentrating benefits among those with robust insurance.
Global Collaboration: Sharing best practices and emerging data to keep pace with evolving gonococcal strains and develop new therapeutic agents or vaccines.
Conclusion
The modest national declines in STI rates are a reminder that with strategic investments and coordinated interventions, progress is possible. DoxyPEP stands out as a promising addition to the prevention toolbox—particularly for chlamydia and syphilis—when backed by sufficient testing, monitoring, and community outreach. Yet the specter of antimicrobial resistance, along with ongoing disparities in healthcare access, underscores that a single biomedical solution must be carefully managed.
Findings from San Francisco and Kaiser Permanente prove doxyPEP can effectively reduce STI incidence in real-world settings. Whether it remains a durable tool will depend on collective commitment: policymakers must fund surveillance and outreach, clinicians must practice stewardship, and communities must engage to ensure equitable access. If implemented wisely, doxyPEP could shape a future where the burden of STIs—and the inequalities that fuel them—diminish, showcasing how targeted prevention strategies can enhance public health without jeopardizing our arsenal of antibiotics.
Partisan Battles Put Public Health Programs in Jeopardy
Federal support for public health programs stood at a critical inflection point in 2024, with mounting evidence that political polarization threatens to undermine decades of progress in disease prevention and healthcare access. The O'Neill Institute's analysis of the HIV response highlights a broader pattern affecting America's entire public health infrastructure: an erosion of bipartisan cooperation is creating tangible negative impacts on healthcare delivery and outcomes.
Recent developments illustrate this crisis. The President's Emergency Plan for AIDS Relief (PEPFAR), historically celebrated as one of the most successful public health initiatives in U.S. history, received only a one-year reauthorization in March 2024 instead of its traditional five-year renewal. This shortened timeframe introduces uncertainty for partner countries and threatens program stability. Similarly, Tennessee's rejection of $8.3 million in Centers for Disease Control and Prevention (CDC) HIV prevention funding exemplifies how state-level political decisions can directly impact public health services and infrastructure.
The implementation of the Inflation Reduction Act (IRA), while advancing certain healthcare affordability goals, has created unintended consequences for safety-net providers. Changes to drug pricing and reimbursement structures are affecting 340B program revenues that support critical healthcare services for vulnerable populations.
These challenges emerge against a backdrop of chronic underfunding, with the Prevention and Public Health Fund losing $12.95 billion between FY 2013-2029. This combination of political polarization and resource constraints threatens to create long-lasting negative impacts on healthcare access and population health outcomes, demanding a renewed commitment to depoliticizing essential public health infrastructure and services.
An Erosion of Bipartisan Support
The deterioration of bipartisan cooperation in public health policy represents a significant shift from historical norms that prioritized health outcomes over political ideology. PEPFAR exemplifies this change. Created under President George W. Bush's administration in 2003, PEPFAR has saved over 25 million lives and currently provides HIV prevention and treatment services to millions across 55 countries. Despite this documented success, the program's 2024 reauthorization became entangled in partisan debates over abortion rights.
"I'm disappointed," Rep. Michael McCaul (R-Texas) stated. "Honestly, I was looking forward to marking up a five-year reauthorization, and now I'm in this abortion debate." McCaul added that "a lot of the Freedom Caucus guys would not want to give aid to Africa." The inclusion of abortion rights in the reauthorization debate reflects ongoing polarization within Congress, which has hindered the passage of traditionally bipartisan public health initiatives. This opposition led to an unprecedented short-term reauthorization through March 2025, creating instability for partner countries and threatening program sustainability.
At the state level, Tennessee's decision to reject $8.3 million in CDC HIV prevention funding reflects similar political calculations overshadowing public health considerations. The state's choice to forgo federal support impacts disease surveillance, testing services, and prevention programs that serve people living with HIV and those at risk of acquiring HIV. This rejection of federal funding occurred despite Tennessee ranking 7th among U.S. states for new HIV diagnoses in 2022.
Such decisions mark a stark departure from historical bipartisan support for public health initiatives. Previous health emergencies, from polio to the early HIV epidemic, generated collaborative responses across party lines. The Ryan White HIV/AIDS Program, established in 1990, exemplified this approach, receiving consistent bipartisan support for reauthorization until 2009, its last reauthorization.
The shift away from bipartisan cooperation extends beyond specific programs to affect broader global health initiatives. PEPFAR's instability impacts America's global health leadership position and threatens the progress made in HIV prevention and treatment worldwide. The program's uncertain future affects procurement planning, workforce retention, and long-term strategy development in partner countries, potentially reversing decades of progress in global health security.
Funding Crisis and Infrastructure Impacts
The public health funding landscape reveals a pattern of chronic underinvestment that threatens core infrastructure capabilities. The Prevention and Public Health Fund (PPHF), established under Section 4002 of the Patient Protection and Affordable Care Act of 2010 (ACA) to provide sustained investment in prevention and public health programs, has lost $12.95 billion between FY 2013-2029 through repeated cuts and diversions. These reductions represent approximately one-third of the fund's originally allocated $33 billion, significantly limiting its ability to support essential public health services.
The CDC faces mounting infrastructure challenges due to stagnant funding. While COVID-19 response funds provided temporary relief, these emergency appropriations have been largely obligated or rescinded. The Fiscal Responsibility Act of 2023 rescinded approximately $13.2 billion in emergency response funding from public health agencies, including the CDC, creating a significant funding cliff. Programs facing severe reductions include the Advanced Molecular Detection program, which will revert to its annual base appropriation of $40 million from a one-time supplemental of $1.7 billion, severely limiting disease surveillance capabilities.
State-level impacts manifest in critical staffing shortages and outdated systems. Public health experts estimate that state and local health departments need to increase their workforce by nearly 80%, requiring an additional 26,000 full-time positions at the state level and 54,000 at the local level. The National Wastewater Surveillance System, crucial for early detection of disease outbreaks, faces reduction from $500 million in supplemental funding to a proposed $20 million in FY 2025, threatening its operational viability.
These funding constraints create cascading effects across the public health system. The Public Health Infrastructure Grant program, which has awarded $4.35 billion to strengthen foundational capabilities across 107 state, territorial, and local health departments, expires in FY 2027 without a clear sustainability plan. Similarly, the Bridge Access Program, ensuring COVID-19 vaccine access for 25-30 million adults without health insurance, ended in August 2024, leaving millions without access to updated vaccines. These funding cuts have significantly curtailed prevention services, limiting the CDC's ability to maintain disease surveillance systems and provide timely interventions.
Healthcare Access and Safety Net Impacts
The implementation of the Inflation Reduction Act (IRA) has created unintended consequences for safety-net providers, particularly through its impact on the 340B Drug Pricing Program. Research examining 340B-eligible hospitals reveals concerning trends in charity care provision, with only 9 out of 38 hospitals (23.7%) reporting increases in charity care as a percentage of annual revenues after gaining 340B eligibility. This decline in charity care occurs despite significant revenue increases from 340B participation, raising questions about program effectiveness in expanding healthcare access for vulnerable populations.
Data indicates that hospital participation in the 340B program correlates with substantial revenue growth but diminishing charity care services. The average decrease in charity care provision as a percentage of annual revenues was 14.79% across examined hospitals. This trend is particularly concerning in states with high poverty rates. For example, three West Virginia hospitals—Cabell-Huntington Hospital, Pleasant Valley Hospitals, and Charleston Area Medical Center—reported some of the largest decreases in charity care despite serving a state where 28.1% of people earn less than 150% of the Federal Poverty Level.
Federally Qualified Health Centers (FQHCs) face unique challenges under these changing dynamics. Unlike hospitals, FQHCs must reinvest every 340B dollar earned into patient care or operations to maximize access. However, the IRA's implementation of Medicare drug price negotiations and insulin cost caps affects the rebate calculations that support these reinvestments, potentially reducing available resources for patient care.
Medication access challenges extend beyond 340B implications. Pharmacy Benefit Managers (PBMs) have responded to IRA provisions by adjusting formularies, sometimes excluding medications that previously generated significant rebates. This particularly impacts insulin coverage, where certain products have been dropped from formularies despite the IRA's intent to improve insulin affordability. These decisions create new barriers to medication access for people who rely on safety-net providers for healthcare services.
Public Health Consequences
The convergence of political polarization and funding constraints creates measurable negative impacts on disease prevention efforts, weakening the capacity of public health systems to effectively address emerging and ongoing health threats. Data from the CDC shows that despite a 12% decrease in new HIV diagnoses over the past five years, driven largely by a 30% reduction among young people, progress in reducing new infections has stalled. The lack of sufficient funding, compounded by political challenges, has limited the capacity to expand prevention services, enhance outreach, and maintain necessary treatment programs. The 31,800 new HIV diagnoses reported in 2022 highlight how flat funding and political barriers have hindered further advances. These barriers prevent scaling up successful prevention strategies, limit access to innovative treatments, and constrain efforts to address disparities in vulnerable communities. Notably, significant disparities persist, particularly among gay men across all racial and ethnic groups, transgender women, Black people, and Latino people. These populations continue to face systemic barriers to healthcare access, stigma, and a lack of targeted resources, all of which contribute to ongoing inequities in health outcomes.
Vaccine hesitancy, intensified by political division, threatens population health outcomes. The CDC reports that routine vaccination rates for kindergarten-age children have not returned to pre-pandemic levels, while exemption claims have increased. Nearly three-quarters of states failed to meet the federal target vaccination rate of 95% for measles, mumps, and rubella during the 2022-23 school year, increasing outbreak risks.
Health disparities are exacerbated when political decisions override public health considerations. Tennessee's rejection of CDC funding exemplifies how political choices can disproportionately impact communities already experiencing health inequities by reducing access to essential prevention and treatment services. Such decisions particularly affect regions where HIV rates among transgender women increased by 25%, and Latino gay men now account for 39% of all HIV diagnoses among men who have sex with men.
Community health center sustainability faces mounting challenges as funding mechanisms become increasingly unstable. The expiration of COVID-19 emergency funding, combined with uncertain 340B revenues and growing workforce shortages, threatens these essential safety-net providers. Public health experts estimate an 80% workforce gap in state and local health departments, hampering their ability to deliver essential services and respond to emerging health threats.
Uncertain Future Under New Administration
With Donald Trump’s return to the White House, the future of the nation's public health programs remains uncertain. The president-elect’s stance on health policy has historically emphasized deregulation, work requirements, and reductions in safety net programs, and early indications suggest a continuation of these priorities.
The new administration is poised to bring changes that could scale back Medicaid, reduce the Affordable Care Act’s consumer protections, and restrict reproductive health access—all of which have the potential to exacerbate existing health inequities and widen the gap in healthcare access for marginalized populations. Furthermore, the inclusion of vaccine skeptic Robert F. Kennedy Jr. among Trump’s advisors could undermine public confidence in vaccination campaigns and other science-backed public health interventions.
Although Trump has not explicitly targeted programs like PEPFAR, the Ryan White Program, or other core public health initiatives, the broader agenda of cutting federal funding and shifting health policy decisions to the state level raises significant concerns. These shifts could ultimately weaken the country’s safety net programs, leading to an increase in uninsured rates and preventable health disparities.
The reemergence of a more partisan approach to healthcare policy, especially one with a focus on cost-cutting and minimal regulatory oversight, risks destabilizing public health progress made over the last several decades. Public health stakeholders—ranging from healthcare providers to patient advocates—will need to prepare for a period of heightened uncertainty and potentially significant changes to the public health landscape.
The coming months will likely determine how public health priorities and programs evolve in this new political era. Advocacy groups, healthcare professionals, and policymakers must remain vigilant and ready to respond as the Trump administration shapes its healthcare policy agenda, one that could either sustain or significantly alter the course of public health in the United States. Such shifts threaten to undermine the nation’s public health stability, with repercussions for healthcare costs, access, and the ability to prevent and control emerging health threats.
New CDC Report; More than a Decade After a Cure, HepC Persists
Last year, the Centers for Disease Control and Prevention (CDC) published a Vital Signs report detailing how “too few people” are being “treated for Hepatitis C” (subtitled: “Reducing Barriers Can Increase Treatment and Save Lives”). Today, the CDC’s landing page reflects a finding from April 2020 that reads “dramatic increases in Hepatitis C” (subtitled: “CDC now recommends hepatitis C testing for all adults”). And in late June, the CDC published a new Morbidity and Mortality Weekly Report (MMWR) on a worryingly low rate of HCV clearance in the United States.
Our previous blog reviewed last year’s report under the lens of health disparities highlighted by researchers’ review of 48,000 patient charts that met the inclusion criteria for the analysis. Then, much like in this new report, identified that lack of curative treatment access was not uniform and was largely informed by the type of insurance patients qualified for. Those payer types (Medicaid, Medicare, and Commercial plans) also represent patients from different backgrounds – meaning different socio-economic statuses, different genders and racial backgrounds – with different outcomes. Overall, Medicaid recipients were only ever prescribed curative treatment about 23% of the time, whereas Commercial payer patients were able to see that rate increase to 35%. The CDC also recognized these payers, and the politicians who set the public policy of Medicaid, represent incredibly tangible barriers via administrative processes, like prior authorization, and policy barriers, like requiring sobriety, a high level of liver damage, or other restrictions to gaining access to curative treatments.
For this year’s report, researchers partnered with Quest Diagnostics to review the viral clearance (or cure) of approximately 1 million patients with an initial infection (Quest provided data for 1.7 million patients with evidence of a history of HCV during the direct acting agents era, or from January 1, 2013 – December 31, 2022). Based on an estimated 2.4 million people in the United States with HCV, this sample represents about 43% of those believed to have experienced an HCV infection in this time frame. This is noted as a limitation in the data, in part, because it only represents data from one commercial laboratory. Though, reasonable observers can make certain conclusions from this data.
Now, we should also note, only about 88% of the 1.7 million patients identified as having evidence of HCV infection ever had received testing and, of those, 69% were identified as having an initial infection. This means the majority of patients identified were newly diagnosed and not facing a chronic HCV infection. Of those, about 7% of patients showed evidence of viral persistence.
Authors note “These findings reveal substantial missed opportunities to diagnose, treat, and prevent Hepatitis C in the United States.”
Coverage was highest among those enrolled in commercial insurance (50%) and lowest in Medicare and Medicaid (8% and 9%, respectively). Particularly startling in the differences between payer types was the prevalence of viral testing; those with an unspecified payor type were screened at about 79% and those with commercial insurance or Medicare had a testing prevalence of about 91%.
Patients with “other”, “unspecified”, or Medicaid as their insurance or payer had showed a lower viral clearance rate (23%, 33% and 31% respectively) than their counterparts enrolled in Medicare or commercial plans (40% and 45%, respectively). Overall, the cure rate was about 34%.
The age range with the highest rate of HCV diagnoses was 40-59 years, representing about 43% of the patient records reviewed. 60% were identified in their charts as male. However, the highest rate of viral clearance was among those aged over 60 and the lowest was for those aged between 20-29 years.
Other limitations to the data include a lack of uniformity in the follow-up period between testing, which might lead to some difference in rates. Similarly, patients might use or be referred to a different lab for follow-ups. Though, the data also does not follow patients and would not capture any representation of subsequent reinfection and cannot make any assumptions as to clearance or viral persistence among those who did not have RNA testing (and referral for treatment) – meaning the data likely underestimates the patients in each of these categories.
Advocates can look toward these data and findings to inform necessary policy changes, particularly by payer type and in seeking appropriate provider activation on screening and treatment. The sheer reality is HCV is both preventable and curable and policymakers and payers need to work more efficiently in order to prevent the approximate 14,000 HCV related deaths this country faces annually.
Opioid Settlements in America
In 2021, a group of state State Attorneys General announced a $26-billion national opioid settlement with three of the largest drug distributors—McKesson Corp., Cardinal Health, Inc., and AmerisourceBergen Corp.—and drugmaker Johnson & Johnson that would see $21b and $5b from those groups, respectively. This settlement deal was approved by all but four states—Alabama, Oklahoma, West Virginia, and Washington—and distribution of those funds began in 2022.
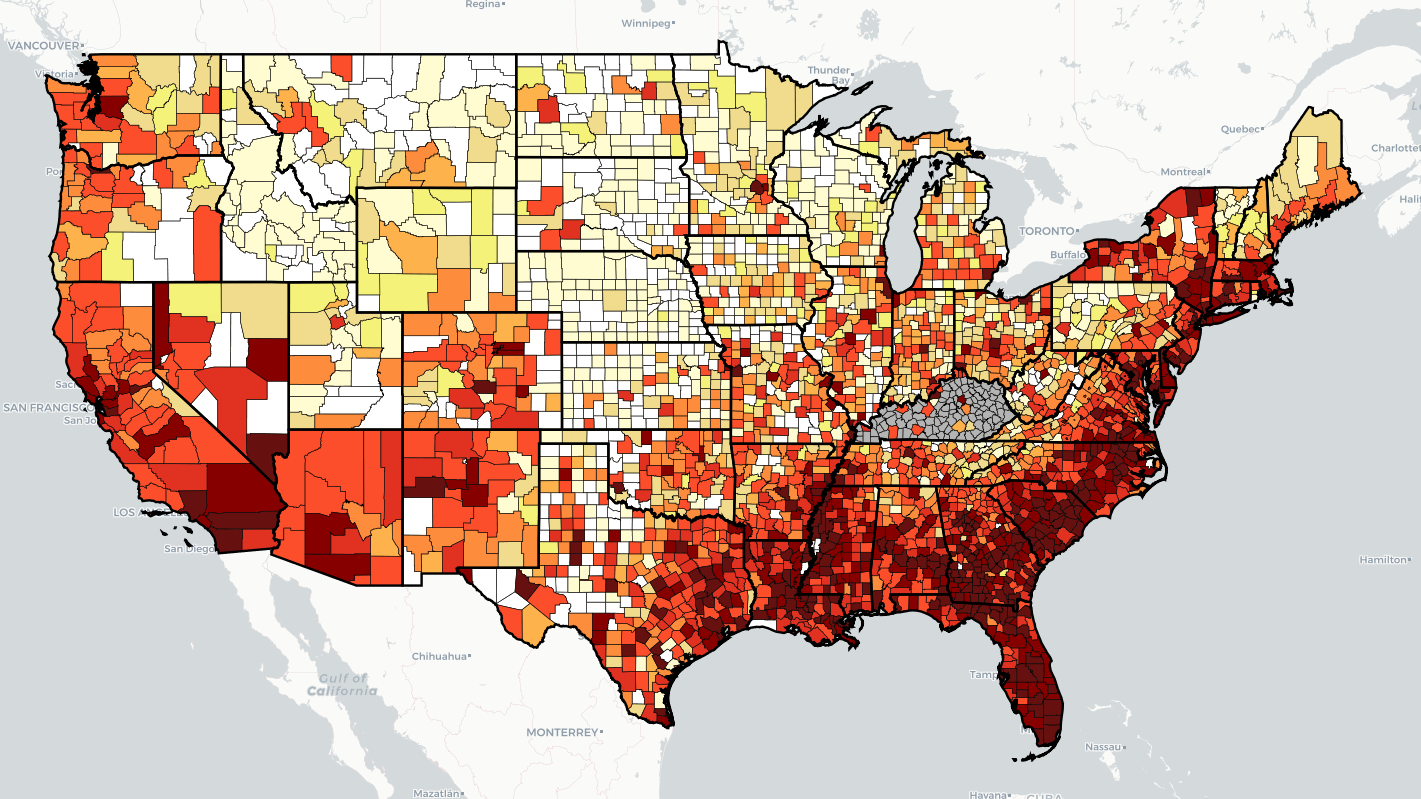
As with every such settlement, funds are distributed to states and municipalities, but how those funds are used is largely up to the recipients. One of the primary critiques of the 1998 Tobacco Master Settlement Agreement was that states and municipalities could use the settlement funds for any purpose. Many states, including West Virginia, used (and abused) those funds to plug holes in their budgets, fund infrastructure improvements, and, in the case of West Virginia, fund teacher pension funds. This lack of direction and oversight meant that relatively few funds actually went to provide healthcare, cessation, or prevention services. Despite this, adult smoking rates have largely plummeted since 1998 but remain relatively high in Appalachian and Midwestern states (Figure 1).
Figure 1 – Current Cigarette Use Among Adults (Behavior Risk Factor Surveillance System) 2019
Source: Centers for Disease Control and Prevention. (2021, October 22). Map of Current Cigarette Use Among Adults. https://www.cdc.gov/statesystem/cigaretteuseadult.html
Negotiators appear to have learned from that mistake, and the National Opioid Settlement is different. However, while the settlement agreement requires that 85% of the funds going directly to states and municipalities must be used for “…abatement of the opioid epidemic,” the settlement doesn’t go so far as to enumerate what qualifies as “abatement.”
According to Kaiser Family Foundation reporting, funds from the settlement are split between states and are then divided in varying percentages across state agencies, local governments, and councils that oversee opioid abatement trusts. But, there has been little transparency around the settlements, including how much each state is received, how those funds are then divided, and how those funds will be used. To date, just 15 states (Arizona, Colorado, Connecticut, Delaware, Florida, Idaho, Massachusetts, Minnesota, Missouri, New Hampshire, New Jersey, North Carolina, Oregon, South Carolina, and Utah) have explicitly promised to report 100% of their Distributor and Johnson & Johnson settlement expenditures. These promises are not, however, legally binding, and recent moves by certain state administrative and legislative bodies to make private information that is statutorily mandated to be public under state Sunshine Laws bode poorly for those hoping to hold states accountable for their use of the funds.
There have been some successful efforts to track the distribution of national settlement funding out of the National Academy for State Health Policy (NASHP). Their map, however, is limited in that it only covers funds from that National Opioid Settlement, meaning that states that chose to continue pursuing additional damages (i.e., West Virginia, Alabama, Oklahoma, and Washington) are not tracked on the map. In addition to the interact map, NASHP provides a pretty comprehensive breakdown of how each state is using opioid settlement funds, including those states that did not participate in the national settlement.
Because we’re still in the early days of the settlement disbursements, there’s not really a great way to measure whether or not the funds will be successfully utilized, nor whether or not the abatement programs will actually have an impact. What we have seen outside of the settlement is that there is little consensus between states on how best to approach the continuing opioid epidemic. While some states increased access to harm reduction services, others have reduced access to, heavily regulated, or eliminated those services altogether.
In states where the opioid epidemic has become part of the fabric of life, such as Indiana, Kentucky, Ohio, and West Virginia, anecdotal reports and some limited research have found that, while additional and public health professionals are actively attempting to implement policies, plans, and interventions to openly and positively confront the opioid crisis, state residents are simply exhausted after dealing with over twenty years of devastation, loss, and both perceived and real destruction to their ways of life.
On the anecdotal front, I recently returned to Eleanor, WV, where I briefly lived and attended school and where my father taught music. What I found made my heart ache: the town’s lone shopping center essentially abandoned and left in disrepair; a middle school whose track and football field (which are still actively used by students) so destroyed that the track was little more than broken concrete loosely interspersed between fields of overgrown grass and bleachers literally tilting from rust and overuse; a set of buildings that once served as some of the town’s few apartment buildings literally burned out and boarded up with graffiti-covered plyboard; school bus stops that looked like they’d been hit by a tornado, and nobody repaired them.
We’re not talking about a major metropolitan area—we’re talking about a town of just over 1,500 residents that carries the moniker, “The Cleanest Town in West Virginia.” And the devastation didn’t stop there. I spent the next hour or so driving along the routes I used to travel as a kid and teenager, and every place that once held a great memory for me was absolutely destroyed or so badly damaged as to be wholly unrecognizable.
When I go through Facebook to check on friends from my time in Eleanor, a significant percentage of them are either recovering, in active use, or have lost their lives to the opioid epidemic. Even after working in the public health and advocacy space for more than fifteen years, the realities sometimes feel remote, and this drive allowed me to see what the opioid epidemic has done to West Virginia: it has deprived us of hope that things can or will get better. What’s more, our state legislature seems determined to make things worse.
These are the states and towns where opioid settlement funds are desperately needed, but it’s unclear whether or not they will receive or utilize them well. I know that I will be actively following how these funds are used in Appalachia, particularly in my capacity as Founder and Executive Director of the Appalachian Learning Initiative (APPLI, pronounced like “apply”).
Australia is on Track to End HIV…by Focusing on Treatment
Last week, researchers funded by the National Health and Medical Research Council of Australia published an assessment of Australia’s success in combatting HIV and how the country might meet its goals to end their domestic HIV epidemic. The study is remarkable in many ways and readers should be cautioned to appreciate the various differences in dynamics between the epidemic in their country of residence and Australia. For example, Australia has been willing to get creative with its policy and program environment and infrastructure to address barriers to care – something many other countries, including the United States, might face steeper challenges in doing.
The study, which focused itself in New South Wales and Victoria – the country’s most populous states. While these areas hold large urban populations, Melbourne and Sidney for example, they also have large rural geographies as they get closer to the interior of the country. This isn’t dissimilar to much of the United States, where the coasts and land boarders, to a lesser degree, are well populated and as you get closer to the interior of the country, that population becomes more rural. Rural and urban geographies present very unique dynamics in and of themselves. And those differences should be well-appreciated when considering the findings of the study.
Specifically, the study sought to assess “whether treatment-as-prevention could achieve population-level reductions in HIV incidence among gay, bisexual, and other men who have sex with men (GBM)”.
What’s most interesting about the study – though not necessarily surprising given historical evidence – is it found a positive correlation between increasing viral load suppression and reduction of new HIV diagnoses. But it’s not a 1-to-1 ration. The study found a 1% increase in viral load suppression was associated with a WHOPPING 6% decrease in new diagnoses. That’s not all folks – that decrease was AFTER an adjustment to account for pre-exposure prophylaxis (PrEP), meaning the 1-to-6 correlation between increased viral load suppression and reduction of new diagnoses was INDEPENDENT of PrEP uptake and use.
Now, that’s not bash PrEP. Rather, the authors argue that to achieve maximum benefit, PrEP should continue to be partnered with our understanding of treatment-as-prevention, or, as messaging goes, Undetectable Equals Untransmittable (U=U). Indeed, the data from the study spans 10 years, which means the authors were able to positively demonstrate how PrEP increases the successes related to treatment-as-prevention.
Authors conclude their work with a direct interpretation: “Our results suggest that further investment in HIV treatment, especially alongside PrEP, can improve public health by reducing HIV incidence among BGM.”
This work is especially important as the United States begins considering a nationalized PrEP program and making exceptional investments in doing so. This study very specifically reminds us that we will NOT reach our goal of ending the HIV Epidemic with PrEP alone…but we might with treatment-as-prevention. And if we were forced to do so with treatment alone, we might still get there if we could overcome barriers to care like stigma, unnecessary barriers to care like utilization management practices, employers leveraging their power in the private market, meeting people where they physically are, closing gaps between “available” and “accessible”, overcoming discriminatory actions aimed at harming those already most affected by HIV, and more.
There’s another advantage in not moving onto PrEP with a near exclusive fervor, HIV treatment is directly life-saving. It is the humanitarian and right thing to do to ensure people already living with HIV are receiving the care and treatment and resources and support we need to thrive.
Directly, this data shows us that we will not defeat HIV by only focusing on people not already living with HIV. Rather we must ensure the lion’s share of our work focuses on people already living with HIV.
There’s much work to do and much promise on the horizon.
I’ll leave advocates with this and a request to search internally.
In December, HBO will be releasing a documentary on the Honorable Nancy Pelosi. The trailer for it is out already. In one clip, one quote, Representative Pelosi, one of our dearest champions, summarizes where our work should guide us, “I came here to do a job, not keep one.”
A Pox in the Hen House: A Timeline of the MPV Outbreak and Topline Numbers
The first Monkeypox (MPV) diagnosis in the United States was reported on May 17th, 2022, though testing data indicate that the first test that returned a positive result was administered on May 10th. By July 3rd, 2022, there were over 1,500 reported cases in the United States.
By early July 2022, white Americans accounted for 47.6% of MPV diagnoses. But by July 24th, 2022, with 7,266 cumulative MPV diagnoses, Black Americans for the first time accounted for most positive diagnoses—32.6%—in the Centers for Disease Control and Prevention (CDC)’s Morbidity and Mortality Weekly Report (MMWR) Week 30. For all but 8 out of the following 28 weeks (ending in MMRW Week 5, 2023), Black Americans accounted for the highest percentage of positive test results. White Americans accounted for the majority of weekly positive diagnoses in only 7 weeks in that same period of time. On August 9th, 2022, the U.S. government declared MPV a Public Health Emergency (PHE). As of February 15th, 2023, there have been a total of 30,193 identified MPV diagnoses and 38 confirmed deaths as a result of MPV.
On May 22nd, 2022, the first JYNNEOS vaccines were administered as prophylaxis against MPV in the United States. Initial supplies of the MPV vaccine were low, however, and the U.S. Food and Drug Administration (FDA), to increase the available supply, issued an Emergency Use Authorization (EUA) on August 9th, 2022, allowing healthcare providers to administer the vaccine in a two-dose series using intradermal administration based on findings from a 2015 study that evaluated the efficacy of intradermal compared to subcutaneous vaccine administration. The total number of vaccines administered in a single week peaked in the week of August 7th – August 14th, 2022, with 108,895 total vaccines administered. By September 10th, 2022, the number of weekly second doses administered outstripped the number of first doses for the first time. This trend continued until the week ending on January 28th, 2023. The number of weekly vaccine administrations dropped precipitously in the week ending on October 1st, 2022. As of February 28th, 2023, a total of 1,196,047 doses of the MPV vaccine have been administered.
Access to and administration of the MPV JYNNEOS vaccine in the United States appear to have been highly correlated to race. In both First- and Second-Dose administration phases, white Americans were the most likely to be vaccinated, with 46.4% of first doses and 50.3% of second doses being administered to white Americans. White Americans received 47.9% of all vaccines administered. Despite the fact that Black Americans represented the highest percentage of diagnoses in the United States—33.7%—just 11.3% of first doses and 10.7% of second doses were administered to Black Americans, receiving just 11.1% of all vaccines administered. Among Hispanic Americans—who accounted for 29.6% of all MPV diagnoses in the United States.—just 20.7% of first doses, 19.6% of second doses, and 20.3% of total doses were administered to this population.
The first doses of TPOXX (tecovirimat) for the treatment of severe MPV disease were prescribed on May 28th, 2022. TPOXX administration is primarily reserved for patients with severe symptoms of the disease, who are immunocompromised, or who have other concurrent conditions that may present complications. As of January 25th, 2023, 6,832 patients were prescribed or treated with TPOXX.
On November 28th, 2022, the World Health Organization (WHO), to address racist and stigmatizing language associated with MPV recommended a global name change for the virus to “MPOX.” (Disclaimer: CANN continues to use “MPV” for its current project merely for the purpose of consistency in report language, but will begin using “MPOX” upon conclusion of the project)
On December 3rd, 2022, the U.S. government announced that it would not be renewing the PHE for MPV. The PHE officially expired on January 31st, 2023.
The Lessons We Applied, the Ones We Learned, and the Ones We Failed to Heed
One of the most successfully applied lessons was the implementation and utilization of existing testing, vaccination, and surveillance systems that were created in response to the COVID-19 outbreak.
Of the 57 reporting U.S. jurisdictions, 31 utilized their existing disease response, reporting, and tracking infrastructures to deploy in-depth disease MPV surveillance for the majority of the outbreak. The surveillance staff and protocols developed during the COVID-19 pandemic quickly pivoted to include MPV in their work, expanding their disease reporting and dashboards to include MPV case counts and demographics to better track the outbreak. Existing vaccine infrastructures including, but not limited to, staffing, scheduling systems, and drive-through delivery spots, were adapted, expanded, or repurposed to incorporate MPV vaccine supplies and dose administration.
Several jurisdictions truly set standards in their reporting, including the states of California, Colorado, Georgia, Kentucky, Massachusetts, Michigan, and New York City (which is reported separately from New York state). They provided excellent MPV diagnosis demographic breakdowns that included age groups, racial/ethnic minority categories, and gender reporting that included trans, non-binary, and other gender expression categories. These data helped to direct responses and better measure equitable outreach, education, and access to treatment and vaccines to the most affected communities.
To hear state and federal public health officials tell it, the U.S. response to the MPV outbreak has been a masterclass in how to effectively respond to and control an epidemic of a highly infectious disease. We’ve heard about how successful and swift the response to the outbreak was and, for a certain segment of the population, that may be true.
For many white, cisgender men who have sex with men (MSM), the outbreak has been little more than a month-long inconvenience; a blip that barely pinged their radars. The other side of that story, however, lies in the marginalized demographic groups.
For all of the successfully deployed public health systems, the truth is that MPV has been almost exclusively a disease that impacts the “others” in our society. From the beginning of the response, LGBTQ+ patients reported facing stigmatizing, discriminatory, and/or outright racist attitudes and behaviors on the part of medical professionals and administrative staff, particularly those seeking services outside of urban settings.
The unfortunate truth of healthcare provision is that every disease that is primarily acquired via sexual transmission comes with its own set of social, moral, and medical stigmata. In areas where self-reported levels of religiosity are high, patients seeking care often encounter negative behaviors and reactions from healthcare workers and administrative staff both inside and outside of the STD/STI/HIV spaces. While the Health Insurance Portability and Accountability Act (HIPAA) is supposed to protect patients, the reality on the ground is that healthcare workers can be woefully loose-lipped when it comes to sinking the social ships of the patients who live in small or close-knit communities. Moral judgments are made; stories get told; patients are admonished and made to feel ashamed—the impacts of these behaviors, both short- and long-term, can lead to patients refusing to seek testing or treatment until they feel they absolutely must, to avoid being honest with physicians about their symptoms, or to refuse to seek vaccinations or treatment services to help prevent infection or the further spread of the disease.
When it came to the delivery of MPV vaccines, the splitting of the JYNNEOS vaccine into two doses both created confusion about the efficacy of the vaccine and increased barriers to people wishing to complete the two-dose series. With any vaccine series, the fewer times patients need to schedule or show up for an appointment to receive their shots, the more likely they are to get fully vaccinated. Additionally, the decision to use intradermal vaccine administration as the delivery method—one of the more difficult delivery methods to correctly perform—resulted in reports of unsuccessful attempts at vaccinating individuals, particularly in patients with darker skin. Additional concerns, which were only marginally addressed by later guidance—and inconsistently applied across jurisdictions and providers—included discomfort and scarring, particularly among those prone to keloids. This meant that several patients—mostly Black and Brown—had to have their dose readministered at a later date creating yet another unnecessary barrier to becoming fully vaccinated.
Another factor that negatively impacted the MPV vaccine uptake was the exponential increase in self-reported hesitancy, skepticism, refusal, and beliefs in scientifically and factually inaccurate information about vaccines, in general. One of the worst consequences of the COVID-19 pandemic response was the massive influx of false information about how vaccines are developed and manufactured, what their contents are, their risks and side effects. Those challenges were compounded by misinformation, such as massive government/billionaire/Jewish/Chinese conspiracies to commit every farcical atrocity under the sun – including surreptitiously implanting microchips, giving people mutant magnetic properties, sterilization…you name it, some shadowy organization was allegedly doing it.
Despite these falsehoods being easily disproven within seconds, for many people the burden of proof has never been on the people making the false claims to prove their theories, but on the “experts” to disprove what the neighbor’s cousin’s sister’s oldest great-grand-nephew said about how the vaccine caused him to go blind.
Beyond those haphazardly manufactured and too easily consumed lies about vaccines, Black and Brown communities have historically legitimate reasons to distrust the government and medical authorities. Decades of actual and well-documented surreptitious sterilization, non-consensual experimentation, and abuse at the hands of systemically racist medical establishments have resulted in a generational and almost endemic distrust of public health measures, treatments, and authorities in minority communities. Efforts to combat generational hesitancy, avoidance, and distrust are slow-going, taking decades of work to undo or repair the harm that has been done to those communities. Add on top of that steady and relatively unchallenged social, digital, and visual media streams churning out anti-vax conspiracy theories, and that process becomes all the more difficult.
In Black and Hispanic men, as well as in communities of Persons Living With HIV/AIDS (PLWHA), MPV was largely allowed to run rampant, in no small part because of ineffective, lacking, or wholly absent educational, outreach, and vaccination strategies designed to reach those communities. While the work done by Drs. Demetre Daskalakis and David Holland in the Atlanta region and in a handful of other major cities was both highly effective and admirable, reality is that their campaign of taking education, testing, and vaccination drives into large-scale venues, gay cruises, fetish events, and sex clubs simply wasn’t scaled and replicated at the levels needed to truly reach those most in need of services.
One of the lessons that we need to learn from the MPV outbreak is that we need to do a much better job of delivering healthcare services outside of traditional settings and offering healthcare services outside of traditional office hours.
We already know that rural, minority, and LGBTQ+ populations face critical healthcare staffing and service provision shortfalls. The closure of rural clinics and hospitals, as well as healthcare providers who served primarily minority and/or lower-income patient populations, has exacerbated the negative outcomes and barriers that exist in areas with underfunded, little, or non-existent healthcare infrastructures. While the growth of COVID-19-related pop-up services and locations provided hope for improvement, the truth is that those investments were never designed to be long-term, nor were those investments or their implementation welcomed in more conservative parts of the country.
If we want to effectively serve underserved populations, we must think and act outside of the standalone brick-and-mortar healthcare paradigm. The MPV outbreak has shown us that we need to significantly increase local, state, and federal investments in mobile, pop-up, and telehealth healthcare delivery methods and models to meet people where they are. We also need to invest in more community-based providers, service models, and interventions. We need more public-private collaboration design – like the New York City Health Department partnering with the Sisters of Perpetual Indulgence for generating a community experiences feedback system.
Many of the most innovative and successful STD/STI/MPV interventions don’t require patients to come into a standard physical location to access testing, vaccination, and treatment services. They are set up in sex clubs and bars; they show up at concerts, parties, and other big events; they offer services in churches in communities where faith plays an important role in the lives of their patients; they build trust in, develop relationships with, and take mobile units into encampments of people experiencing homelessness. Essentially, they go out and meet patients where they are and when they’re available. A pox in the hen house has taught us one very valuable lesson: we need to fix these barriers sooner rather than later.
When MPV Became An STI
There comes a time, in the progression of any outbreak, where classifications change as we grow to understand more about the disease; a time when people—those who are living with the disease, those who have recovered, those who have never come in contact, and those who encounter the disease in a professional capacity—decide that we’re no longer in the midst of an “outbreak,” but that it has either ended or become endemic. This is where we appear to be with the Monkeypox (MPV) outbreak in the United States.
Since the beginning of the MPV outbreak in the United States, the overwhelming majority of cases have been transmitted via sexual contact (Centers for Disease Control and Prevention, 2022), primarily among men (CDC, 2023), particularly among Men who have Sex with Men (MSM) (Spicknall, et al., 2022), and disproportionately among Black Americans (CDC, 2023). The Community Access National Network (CANN) has been actively tracking reporting of MPV since September of 2022, and in that time, we have witnessed a troubling pattern emerging: the celebration of a “successful” control and suppression of a disease outbreak when the disease actually risks becoming endemic.
When we say that a disease has become endemic, it means that the disease is a constant presence in a certain population within a specific geographic region. In this case, we mean that MPV has relatively rapidly transitioned from a highly concerning outbreak to one that is being treated as a sexually transmitted infection (STI) similar to syphilis—one that is likely going to just “be around” no matter what we do. In the MSM communities that have been overwhelmingly impacted by MPV, members of those communities have already started treating it as such:
“We know it is how we are getting it, we just don’t know what to do about it because, based on lesion location alone, for example, a condom would not have prevented some of these exposures.”
This comment from an HIV activist and advocate living in New York City’s Hell’s Kitchen was related to me during a conversation about anecdotal reporting of disease outbreaks in the area.
“I know of at least a dozen men in the last couple of weeks who are experiencing minor infections despite being vaccinated or previously infected, and this week, I have seen several sex workers in the streets around here who are clearly experiencing full-blown infections, implying no vaccination.”
These statements raise several concerns, not the least of which is the availability of vaccine supplies and the distribution of said vaccine among priority populations. Additional concerns include what, if anything, can be done to curb the spread of MPV among MSM populations when vaccine supplies are unable to keep up with the demand if the virus is, in fact, becoming endemic. Will we simply decide, as a nation, that it’s just something we have to live with and move on with our lives?
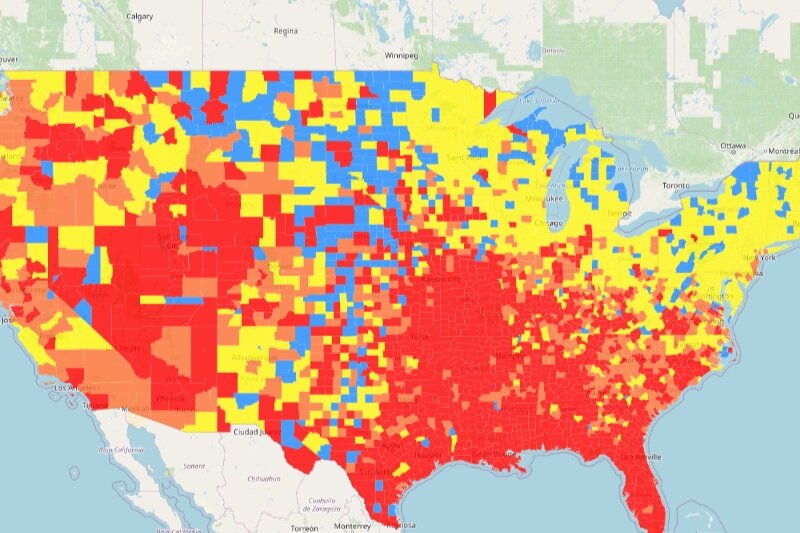
One of the unfortunate truths about the availability and distribution of the MPV vaccine is that the populations who were the most disproportionately impacted by the virus were some of the least likely to receive the vaccine. As of January 19th, 2023, 48.3% of vaccines administered have been administered to White residents, despite the fact that just 22.4% of MPV cases have occurred in White residents. Comparatively, 34.7% of MPV cases have been identified in Hispanic residents, with just 23.4% of vaccines going to that population, and 27.4% of MPV cases have been identified in Black residents, with just 12.8% of vaccines going to that population.
Essentially, vaccination outreach efforts have simply not been sufficient to reach the populations most heavily impacted by the disease. While many factors may contribute to this outcome, the primary factor is that Black and Hispanic Americans simply do not have access to or receive the quantity and quality of care that White Americans enjoy—a fact that has been widely discussed but poorly addressed since the early 2000s (Collins, et al., 2002). From the quality of the facilities and services to the availability of service providers, White Americans are more likely to have access to not just more healthcare services but better services that meet their needs, whereas Black and Brown Americans are made to deal with longer wait times, under-resourced and understaffed facilities, and often lower quality care.
While there certainly have been efforts to reach into Black and Brown communities to deliver the same quantity and quality of healthcare services, healthcare workers come up against cultural barriers, including having to confront the generations of discrimination, mistreatment, and neglect that Black and Brown Americans have faced from healthcare professionals that make those populations less likely to seek healthcare services and trust providers.
These are the same barriers that people working in the HIV and STD/STI fields face when trying to provide services, and we still struggle to overcome those barriers today, although progress is being made, particularly when healthcare services are provided by members of those communities whom they know and trust. The same logic can and should apply to the delivery of vaccines, but the sad reality is that vaccine hesitancy and refusal continue to be high in Black and Brown communities (Maurer, Harris, & Uscher-Pines, 2014).
Beyond racial disparities, further concerns exist around barriers that impact the general MSM, Transgender, and Queer populations. One such barrier is the lack of culturally competent, sex-positive, and queer-centric care provision, even in areas as diverse as Hell’s Kitchen:
“A number of my friends, as well as myself, if I’m being honest, have reported that their physicians are both unaware that reinfection with MPV is possible and that infections can still occur in people who have been fully vaccinated, and as a result of their knowledge gap are refusing to test MPV lesions.” my friend continued. “There is a paucity of physicians who understand that LGBTQ+ people are going to continue to be sexually active, and this lack of cultural competence leads to our critical healthcare needs going unaddressed.”
What many Americans, and sadly many physicians and healthcare providers, fail to recognize is that healthcare is rarely a “one-size-fits-all” provision model. When we talk about diversity in patient populations, we’re should be talking about more than just racial diversity; we need to include sex and gender diversity, sexual orientation diversity, religious diversity, age diversity, and income diversity. Every patient, whether or not they are aware of them, is impacted by a wide variety of experiences related to their race, age, sex, gender, sexual orientation, and religious beliefs, and those experiences inform when, why, and how they access healthcare services. When providers are not aware of and responsive to those experiences—something that is truly difficult, particularly in areas where the patient-to-physician ratios are astronomically high—the quality of the services being provided suffers.
One way to approach this would be the better (and potentially mandated) incorporation and provision of STD/STI testing, prevention, and care in general practice settings. This would help to normalize the testing, identification, and treatment of STD/STIs in the general population and make seeking services for them less stigmatizing.
Another opportunity that is rarely explored is the provision of STI testing and vaccination services in sex-based venues, such as sex clubs, bath houses, and other venues where intimate contact between individuals is likely to occur. While some physicians—most notably Drs. David Holland and Demetre Daskalakis—have been actively pushing for and engaging in this type of health intervention, it is still a relatively rare type of intervention outside of large urban areas. Moreover, providing these types of services requires additional training for staff, particularly around situational and cultural awareness, as well as developing best practices for interacting with people in these types of settings without negatively impacting the atmosphere and customer bases of those settings.
If we are ever going to eradicate MPV in the United States, we are going to have to do a significantly better job of getting vaccine supplies to those most likely to be impacted and do a better job of overcoming the cultural and hesitancy barriers that exist in those communities. It also means that we have to do a better job of educating the MSM community about the virus and how it’s spread and doing so in a way that is both sex-positive and doesn’t rely upon fear-based tactics to scare people into getting vaccinated or into a monastic lifestyle.
More importantly, we need to come up with a way to incorporate anecdotal reporting of localized outbreaks of MPV in communities into our responses. While the CDC and states may be taking victory laps on their “successful” MPV responses, the reality is that MPV outbreaks are still ongoing and, in many places, are doing so relatively unchecked with little awareness of the disease, its symptoms, its treatments, or how to prevent it.
While anecdotal evidence is just that—based on personal experience rather than hard data or research—we know that anecdotal evidence can be very important when it comes to identifying outbreaks early, particularly in minority and underserved communities. We need to develop a better way to incorporate those anecdotal reports into our investigations so that we can catch outbreaks early on rather than waiting until cases become widespread. Simply because official reports of cases show a decrease in new infections doesn’t mean that infections aren’t occurring in populations that are less likely to seek healthcare services.
References
Centers for Disease Control and Prevention. (2022, December 08). How It Spreads. Atlanta, GA: United States Department of Health and Human Services: Centers for Disease Control and Prevention: National Center for Emerging and Zoonotic Infectious Diseases: Division of High-Consequence Pathogens and Pathology. https://www.cdc.gov/poxvirus/monkeypox/if-sick/transmission.html
Centers for Disease Control and Prevention. (2023, January 18). Mpox Cases by Age and Gender, Race/Ethnicity, and Symptoms. Atlanta, GA: United States Department of Health and Human Services: Centers for Disease Control and Prevention: National Center for Emerging and Zoonotic Infectious Diseases: Division of High-Consequence Pathogens and Pathology. https://www.cdc.gov/poxvirus/monkeypox/response/2022/demographics.html
Collins, K.S., Hughes, D.L., Doty, M.M., Ives, B.L., Edwards, J.N., & Tenney, K. (2002, March). DIVERSE COMMUNITIES, COMMON CONCERNS: ASSESSING HEALTH CARE QUALITY FOR MINORITY AMERICANS. The Commonwealth Fund. https://www.commonwealthfund.org/sites/default/files/documents/___media_files_publications_fund_report_2002_mar_diverse_communities__common_concerns__assessing_health_care_quality_for_minority_americans_collins_diversecommun_523_pdf.pdf
Maurer, J., Harris, K.M., & Uscher-Pines, L. (2014). Can routine offering of influenza vaccination in office-based settings reduce racial and ethnic disparities in adult influenza vaccination? Journal of general internal medicine, 29(12), 1624–1630. https://doi.org/10.1007/s11606-014-2965-z
Spicknall, I.H., Pollock, E.D., Clay, P.A., Oster, A.M., Charniga, K., Masters, N., Nakazawa, Y.J., Rainisch, G., Gundlapalli, A.V., & Grift, T.L. (2022, September 02). Modeling the Impact of Sexual Networks in the Transmission of Monkeypox virus Among Gay, Bisexual, and Other Men Who Have Sex With Men — United States, 2022. MMWR Weekly 71(35), 1131-1135. http://dx.doi.org/10.15585/mmwr.mm7135e2
Troubling Issues with HIV and Monkeypox Co-Infection
In the process of gathering state-level data on the incidence and demographics of Monkeypox (MPV) in the United States, we have come across several reports of people who have been diagnosed with MPV being co-infected with HIV. This worrisome trend indicates the need for targeted interventions, increased testing, and better communication about MPV in both patient and provider settings.
The Community Access National Network (CANN) has launched an ambitious patient awareness campaign focused on the ongoing Monkeypox outbreak. Its ‘MPV Response Project for People Living with HIV’ seeks to gather data and issue reports covering MPV in the United States. The reports will focus on epidemiological trends, vaccine access and equity, state-level access to vaccine and antiviral supplies, HIV and MPV co-infection risk and reporting, and the latest news related to the outbreak. The project is broad in scope, and it will tackle the MPV outbreak in a way that is both data-focused and patient-centric. This month’s blog will focus on the disparities faced by people living with HIV/AIDS (PLWHA) and MPV.
Data from the European Union, United Kingdom, and the United States suggest that between 28% and 51% of persons diagnosed with MPV are also living with HIV (Kuehn, 2022). According to estimates from the U.S. Department of Health and Human Services (HHS), an estimated 40% of people who have been diagnosed with MPV in the U.S. are also living with HIV (HIV [dot] gov, 2022).
These data are considerably troublesome, particularly as research is beginning to show that PLWHA are likelier to have worse manifestations of MPV, require hospitalization more frequently than persons who are not living with HIV, and are likelier to die as a result of MPV co-infection.
The underlying issue?
We simply don’t have enough localized data (or really, financial resources) to create strategic responses.
Currently, there are only three major jurisdictions in the U.S. that publicly report on HIV co-infection in MPV diagnoses—Michigan, North Carolina, and Rhode Island. This includes looking at the municipal jurisdictions that were specifically targeted for JYNNEOS vaccine supplies—Los Angeles, Chicago, New York City, and Houston—of which only Los Angeles’ reporting mentions HIV, and even then, only in relation to tecovirimat (TPOXX) prescribing data.
So, what does this mean?
Primarily, it means that we need to look at other sources in order to extrapolate co-infection data and use modeling to make educated guesses about where risks of co-infection are highest and how best to respond.
There are currently only a handful of recent studies and surveys that focus on the United States outbreak of MPV from which we can glean these data:
1. Curran, et al., published in September 2022, focused on a sample of 1,969 from eight jurisdictions:
California
Los Angeles
San Francisco
District of Columbia
Georgia
Illinois
Chicago
New York (excluding New York City)
These jurisdictions were selected because they were independently funded for HIV surveillance and because they represented areas with the highest rates of MPV infections in the United States.
Curran, et al., found that 755 patients (38%) of that sample were co-infected with HIV. Of those patients, 94% had received HIV care in the past year, and 82% were virally suppressed (Curran, et al., 2022).
2. Miller, et al., released in October 2022, looked at a significantly smaller sample size of just 57 patients who had been admitted to hospitals for severe manifestations of MPV.
Of this sample, 47 (82%) were co-infected with HIV, just four of whom (9%) were receiving antiretroviral therapy (ART) to treat their HIV prior to being diagnosed with MPV.
In terms of demographics, 68% of this sample were non-Hispanic Black Americans, which highlights disparities in HIV treatment in Black communities.
Prior to the release of this report, 12 of those patients died. MPV was listed either as the cause of death or a contributing factor in five of those deaths, six deaths remain under investigation to determine if MPV was the cause or a factor, and 1 death was deemed neither the cause nor a contributing factor (Miller, et al., 2022)
So, what can we learn from these relatively limited findings:
1. We can determine that PLWHA, particularly Men who have Sex with Men (MSM), are at higher risk of contracting MPV than their heterosexual or women peers.
From the data we have reported in previous blog posts and the reports we’ve released, MPV infection rates are highest in three primary populations:
a. MSM
b. Black Americans
c. Hispanic Americans
This should lead us to build strategies that focus on education of providers about properly identifying MPV lesions, testing, vaccination, and treatment of MPV in these communities.
An additional consideration is a lack of uniformity in gender identity reporting and data collections. As of current, while some jurisdictions are collecting gender identity data for MPV metrics (with many more getting a much better handle on the same data for HIV-related metrics), most are not. Similar to data collection and reporting in HIV prior to about 2016, MPV data does not typically distinguish between a person’s sex assigned at birth and gender identity, thus not adequately capturing data that would appropriately represent transgender communities.
In our gathering of state-level MPV reporting, we found that 22 of the 32 jurisdictions that provide gender demographic reporting either do not report on transgender patient populations, at all, or lump all non-cisgender patients into an “Other” category that fails to capture the diversity of patient populations and health outcomes between them.
Two examples of how this data delineation proves particularly relevant can be observed in the emergence of information regarding HIV prevalence among transgender women, particularly transgender women of color, and, more recently, transgender men have largely been ignored as a target population, likely because of stereotypes and assumptions as to the types of sexual activity transgender men might engage in and because transgender men are less likely to access care (Demmons, 2019). A recent study conducted by AIDS United highlighted how deeply flawed some of those assumptions are, with 35% of the transgender men responding to the survey with a self-reported HIV-positive status (AIDS United, 2022).
Further consideration should also be given to persons experiencing or at risk of experiencing homelessness. Miller, et al., found that 23% of the admitted patients were experiencing homelessness, which is likely indicative of a growing outbreak among a key population: PLWHA who may be housing insecure.
2. We don’t know what we don’t know.
One of the largest concerns, here, is that a majority of providers in the United States simply aren’t familiar enough with MPV to identify the disease consistently and correctly. Since the beginning of the epidemic, physicians have struggled to do so, with many misdiagnosing MPV as other diseases or infections, such as herpes or syphilis (Doucleff, 2022). This is because both of those sexually transmitted infections may manifest as skin lesions, similar to MPV. Misdiagnosis can lead to both the provision of ineffective treatments and result in the unchecked spread of MPV. This highlights the need for better provider education about MPV, its manifestations, and how to correctly differentiate between various diseases.
Additionally, while both Curran and Miller provide reporting on HIV co-infection in persons diagnosed with MPV, none of the listed jurisdictions from which they selected their sample groups provide public-facing reporting on HIV co-infection.
In the three jurisdictions we found with this reporting—Michigan, North Carolina, and Rhode Island—48.6% of MPV patients were co-infected in Michigan, 51.6% in North Carolina, and 27.7% in Rhode Island.
These findings fall relatively neatly into the HIV.gov reporting that 28% - 52% of MPV patients are likely to be co-infected with HIV.
However, these numbers could potentially be higher, particularly in major cities, such as Los Angeles, San Francisco, Chicago, New York, DC, Atlanta, and other areas that have higher populations of PLWHA and more areas and venues where PLWHA tend to congregate (e.g., bars, restaurants, sex clubs, steam rooms, et cetera).
3. Although overall diagnoses of MPV have fallen precipitously since August 2022, there is a significant risk of MPV becoming endemic in MSM, LGBTQ, and PLWHA populations.
This will require the development and wider distribution of better MPV-specific vaccines, better MPV-specific treatments, and better education and health communication about MPV and its transmissibility.
There seems to be a prevailing belief that the United States has weathered the worst of MPV. With declining positivity rates, there are some in the public health community who have decided that resources and attention would be better spent elsewhere—specifically, they’re looking at the tridemic of COVID-19, influenza, and respiratory syncytial virus (RSV) that is leaving hospitals once again scrambling for ICU beds. More accurately, it may be said that jurisdictions either cannot or will not expand the existing resources and personnel to allow for the continued surveillance of MPV. This essentially relegates the work of focusing on, addressing, and frankly caring about MPV to those working in HIV and infectious disease spaces.
Already, we are seeing this trend in data reporting: the state of Texas has removed MPV data entirely from its data dashboard, replacing it with Multisystem Inflammatory Syndrome in Children (MIS-C). This is indicative that a lack of financial and human resources, or the lack of political will or interest to increase those resources, will force state departments of health to reduce reporting on MPV in favor of diseases that impact populations they deem “more important” than MSM, Black, and Hispanic populations.
This, again, raises the concern that MPV will become a virus that is all but forgotten by the general public and general practitioners, as those who face the greatest impacts are already marginalized populations. The disparities faced by those bearing the brunt of MPV mirror those in new HIV diagnoses; it is incumbent upon us to respond evaluate and respond to those trends accordingly.
References
AIDS United. (2022, November). CHANGING THE GAME: Visibility of Trans Men in the South. Washington, DC: AIDS United: News and Resources. https://aidsunited.org/wp-content/uploads/2022/11/ChangingTheGame-FinalReport.pdf
Curran, K.G., Eberly, K., Russell, O.O., et al. (2022, September 09). HIV and Sexually Transmitted Infections Among Persons with Monkeypox — Eight U.S. Jurisdictions, May 17–July 22, 2022. MMWR Weekly 71(36), 1141-1147. http://dx.doi.org/10.15585/mmwr.mm7136a1
Demmons, S. (2019, July 10. Why are trans men invisible in HIV prevention & care? San Francisco, CA: San Francisco AIDS Foundation: Our Voices. https://www.sfaf.org/collections/beta/why-are-trans-men-invisible-in-hiv-prevention-care/
Doucleff, M. (2022, June 06). Monkeypox cases are going undetected or misdiagnosed. Washington, DC: National Public Radio: All Things Considered. https://www.npr.org/2022/06/06/1103372564/monkeypox-cases-are-going-undetected-or-misdiagnosed
HIV [dot] gov. (2022, November 30). mpox and People with HIV. Washington, DC: United States Department of Health and Human Services: Office of Infectious Disease and HIV/AIDS Policy: HIV.gov. https://www.hiv.gov/hiv-basics/staying-in-hiv-care/other-related-health-issues/monkeypox
Kuehn, B. M. (2022, September 27). Interim Guidance for Monkeypox Among Patients With HIV. JAMA 328(12), 1173-1174. https://doi.org/10.1001/jama.2022.14727
Miller, M J., Cash-Goldwasser, S., Marx, G.E., Schrodt, C.A., Kimball, A., Padgett, K., Noe, R.S., McCormick, D.W., et. al. (2022, October 26). Severe Monkeypox in Hospitalized Patients — United States, August 10–October 10, 2022. MMWR ePub. http://dx.doi.org/10.15585/mmwr.mm7144e1
State-Level Monkeypox Surveillance Highlights State-Level Disparities
The Community Access National Network (CANN) launched an ambitious patient awareness campaign focused on the ongoing Monkeypox (MPV) outbreak. Its ‘MPV Response Project for People Living with HIV’ seeks to gather data and issue reports covering MPV in the United States. The reports will focus on epidemiological trends, vaccine access and equity, state-level access to vaccine and antiviral supplies, HIV and MPV co-infection risk and reporting, and the latest news related to the outbreak. The project is broad in scope, and it will tackle the MPV outbreak in a way that is both data-focused and patient-centric. This month’s blog will focus on the demographic disparities of the MPV outbreak, in general, and how those disparities vary at the state level.
The Centers for Disease Control and Prevention (CDC) has been providing considerably detailed data about MPV since the beginning of the outbreak in the U.S. in May 2022. From its MPV data portal, users can get a surprisingly robust amount of national-level data, one of the most striking of which is that Black Americans account for roughly 44% of all new MPV diagnoses across the U.S. (CDC, 2022).
As part of this MPV Response Project, CANN has decided to dig deeper by attempting to gather and analyze state-level epidemiological reporting where it exists. Our experience with state-level surveillance has shown that, while every state has some sort of surveillance system in place, no two systems are created equally. That is to say, while some states provide robust surveillance and reporting, other states—particularly those located in the American South and rural West—do not. More to the point, they likely cannot, as a result of underfunded and understaffed departments.
With this established, here is what we found:
As of October 28th, 2022:
28 states (AL, AR, CA, CO, CT, DE, FL, GA, IL, IN, KY, LA, MD, MA, MI, MN, MS, NJ, NM, NY, NC, RI, SC, TX, VA, WA, & WI) and the District of Columbia provide detailed demographic reporting on Monkeypox virus incidence on state-run websites. Both DE and FL omit race demographics from their reporting.
13 states (HI, ID, IA, KS, ME, MT, ND, OH, OR, SD, TN, UT, & WY) provide case counts, but no demographic breakdowns on state-run websites.
9 states (AK, AZ, MO, NE, NH, OK, PA, VT, & WV) and Puerto Rico report data directly to the CDC with no reporting on state-run websites.
1 state (NV) currently has a reporting dashboard under construction
It was heartening to see that roughly half of the jurisdictions in the U.S. (when including the U.S. territories) provided relatively thorough demographic reporting. This is likely because the data dashboard systems for reporting real-time disease surveillance were already purchased and in place as a result of tracking implemented to report COVID-19 data. 28 states provide some level of demographic reporting, and almost all of those states provide reporting on race.
There are still, however, significant gaps in these data. For example, Florida—one of the most racially diverse states in the U.S.—provides no demographics broken down by race; only by age. This lack of reporting presents a significant barrier to advocates, providers, and legislators because it homogenizes the results. If we are unable to see which populations are disproportionately impacted by MPV—or any disease, for that matter—then how are we to deliver data-driven public health interventions?
An additional issue exists with states’ decisions on how and where they account for Hispanic populations. While some states include “Hispanic” as a separate race category, others treat it as an “Ethnicity” that overlaps multiple race categories. While the latter classification is technically correct—there are Black and White persons who are also Hispanic—this creates a data issue that makes comparing data across states difficult.
In the states with state-level demographic reporting, Black Americans account for a majority of new MPV diagnoses in eleven states (AL, AR, GA, LA, MD, MI, MS, NC, SC, TN, & VA). Of those states, nine are located in the American South, all of which rank in the top ten states with the highest number of Black residents as a percentage of their states’ populations. As an example, in Alabama, Black Americans constitute 26.5% of the state’s population but account for 71% of MPV diagnoses (Alabama NEDSS Base System, 2022). Similarly, in Georgia, Black Americans constitute 32% of the state’s population but account for 77% of MPV diagnoses (Georgia Department of Public Health, 2022).
This is not the case, however, in every jurisdiction. In California, New Jersey, and New York state, Hispanic Americans represent the majority of new MPV diagnoses, as well as in New York City, which is counted as a separate jurisdiction from New York state. Additionally, in Colorado and Massachusetts, while Hispanic Americans do not account for the majority of new diagnoses, they do account for a significantly greater percentage of diagnoses than Black Americans living in those states. In Colorado, Hispanic Americans constitute for 22% of the state’s population but account for 34.8% of MPV diagnoses (Colorado Department of Public Health, 2022). Similarly, in Massachusetts, Hispanic Americans constitute 12.8% of the state’s population but account for 31% of MPV diagnoses (Massachusetts Department of Public Health, 2022).
Unfortunately, in the United States, case surveillance is set at the state level, with each state determining what diseases they track, how they track them, and how they report them. This system, while protected under the 10th Amendment, is more of a liability than an asset. By leaving these decisions in the hands of states, they are infinitely more subject to political machinations by anti-science legislators than were these decisions to be placed under the purview of the Department of Health and Human Services.
Further complicating the inefficiency of our nation’s myriad surveillance systems is that state departments of epidemiology and surveillance must be adequately funded to perform these duties—a feat that, at least at the state level, is becoming less likely given the political makeup of their legislatures. One of the unfortunate impacts of the COVID-19 pandemic’s stellar state-level reporting was that certain political factions have determined that disease surveillance is political, rather than factual; that the science is not to be trusted, because the science is “biased.”
An example of this occurred in West Virginia, in 2021, when state and local legislators, in a public hearing, informed Dr. Demetre Daskalakis, then Director of the Division of HIV/AIDS Prevention at the CDC, that they did not believe him when told that West Virginia’s outbreak of HIV among Persons Who Inject Drugs was worse than in New York City (Peace, 2021). In response to his assertion, the Kanawha County Commission demanded that Senator Joe Manchin submit a congressional inquiry with the CDC to question the validity of his statements (Raby, 2021). This was not an isolated incident; state legislators in Conservative-run states have consistently disregarded and even demonized basic scientific data reporting as if it were a conspiracy against them.
As a result of this increased, and yet paradoxically incurious, scrutiny of disease surveillance, some states are choosing to decrease or drastically cut funding to those departments. And the stark reality is that this trend is likely to get worse before competent heads prevail. In response to what members of one political party have consistently referred to as “government overreach,” at least 20 Conservative-run states used their 2021 legislative sessions to enact new laws that “…preclude the use of proven public health measures or more broadly constrain the authority of state and local health officials, and governors, in a public health crisis” (Vestal, 2021). This means that, even with targeted federal funds, state departments of health and local health officials may be constrained in what they can legally do at the state level. Worse still, many of those state legislators have created committees designed to identify “misspending”—a thinly veiled code for “work we find objectionable”—and to slash budgets to ensure that the “overreach” cannot be implemented, again.
What patients, providers, and advocates can do is reach out to their state and federal legislators to advocate for greater funding specifically for surveillance, and to request that those funds come with stipulations for how they can and cannot be used and when they must be disbursed, so that states do not allow those funds to languish in interest-bearing accounts rather than spending those funds. Additionally, readers can reach out to their states’ departments of health to request that they improve the availability or make available demographic data that are broken down into useful categories that can be turned into direct action to address any disparities these data may identify.
The quest to improve the quality of our data is going to require both federal standard setting and the funds to implement them. Let’s make it happen.
References
Alabama NEDSS Base System. (2022, November 01). What You Need to Know About Monkeypox in Alabama. Alabama Department of Public Health. https://tableau.adph.state.al.us/views/MPXFINALusingextractallsheets/MPXPublic?%3Adisplay_count=n&%3Aembed=y&%3AisGuestRedirectFromVizportal=y&%3Aorigin=viz_share_link&%3AshowAppBanner=false&%3AshowVizHome=n
Centers for Disease Control and Prevention. (2022, October 26). Monkeypox Cases by Age and Gender, Race/Ethnicity, and Symptom. Atlanta, GA: United States Department of Health and Human Services: Centers for Disease Control and Prevention: Poxvirus: Monkeypox. https://www.cdc.gov/poxvirus/monkeypox/response/2022/demographics.html
Colorado Department of Public Health. (2022, October 26). Colorado Monkeypox Data. Colorado Department of Public Health: Diseases A to Z: Monkeypox. https://cdphe.colorado.gov/diseases-a-to-z/monkeypox
Georgia Department of Public Health. (2022, October 26). Georgia Monkeypox Situational Report – October 26, 2022. Georgia Department of Public Health: GA Monkeypox Outbreak Cases and Vaccination. https://dph.georgia.gov/document/document/mpx-situational-report-october-26-2022/download
Massachusetts Department of Public Health. (2022, October 27). Monkeypox Cases and People Vaccinated by Age, Sex and Race/Ethnicity. Massachusetts Department of Public Health: Bureau of Infectious Disease and Laboratory Sciences: Monkeypox. https://www.mass.gov/doc/weekly-report-monkeypox-cases-and-people-vaccinated-october-27-2022/download
Peace, L. (2021, February 11). The CDC says Kanawha County’s HIV outbreak is the most concerning in the United States. Mountain State Spotlight. https://mountainstatespotlight.org/2021/02/11/the-cdc-says-kanawha-countys-hiv-outbreak-is-the-most-concerning-in-the-united-states/
Raby, J. (2021, April 06). CDC inquiry sought on HIV outbreak in Kanawha County. The Parkersburg News & Sentinel. https://www.newsandsentinel.com/news/local-news/2021/04/cdc-inquiry-sought-on-hiv-outbreak-in-kanawha-county/
Vestal, C. (2021, July 29). New State Laws Hamstring Public Health Officials. The Pew Charitable Trusts. https://www.pewtrusts.org/en/research-and-analysis/blogs/stateline/2021/07/29/new-state-laws-hamstring-public-health-officials
HCV ‘Netflix’ Model Reveals Price Isn’t the Biggest Problem
A recent article published to STAT News offers a detailed view on how in 2019, Louisiana and Washington State invested in the headline making, flashy deal of the century. It involved an unlimited supply of direct acting agents (DAAs) known to cure Hepatitis C (HCV) for the price of a standard “subscription” fee. Now, it wasn’t a $9.99 per month, endless video watching gig, but rather thousands of prescription fills per month meant to address the needs of each state’s Medicaid program and correctional facilities. However, such penned deals are estimated to have already saved the two states hundreds of millions of dollars. The subscription model is exciting, STAT reports the Biden Administration wants to build a similar program on the federal level. So that should solve the problem, right?
Not so fast! The data, and the experts, offer a more cautious tone.
A heady launch led to incarcerated people, who had previously sued for access to these curative treatments, finally received them. The states moved to reduce the “utilization” restrictions, like prior authorizations or requirements to have a specialist supervise the care. But that steady progress slowed to a trickle, and signs exist that the progress is already being lost.
2020 brought well-known disruptions in care, including reductions in screenings in hospital settings, and strained prison and jail staffing. And while the COVID-19 pandemic’s crisis phase may provide somewhat of a pass, it doesn’t explain all of the losses and slow return to focus on each state’s plan to eliminate HCV.
What’s at the core of the elimination efforts missing their mark? The planning and implementation of the program hinged on the idea that drug cost was the primary issue as to why people weren’t accessing this curative treatment. Turns out, even if the drug is free to patients and affordable for states, there’s more to care than cost, especially in public health. Despite hundreds of millions in saved dollars, neither state set aside enough (or any) of those projected savings to bolster provider education, invest in the human capital necessary in health care entities serving the most affected public (like federally qualified health centers), or reimbursement for “street medicine”, or innovative program designs, or – as especially is the case in Louisiana – ensuring state health departments have the staff dedicated toward HCV elimination.
Let us take a second to consider that last point. Louisiana’s STI, HIV, and Hepatitis Program is in pretty desperate shape. A long list of job openings reflects the fact that much of the program’s staff are subcontractors with those contracts spread across three different entities, a result supposedly of former Governor Bobby Jindal’s efforts to gut the program entirely, the program can’t attract or retain talent because wages remain ridiculously uncompetitive and, in instances where staff is offered promotions, they have to consider the trade off of losing their health benefits and accrued vacation days for a short period of time if that position is being held under one of the other three contracts. With that kind of tangled web to navigate, no wonder the state is falling behind. On social media, some state legislators have openly mocked the Louisiana Department of Health asking for budget increases. None of that touches the lack of physical access points of care patients need in more rural parts of the state – sometimes driving hours to find a provider to treat their HCV – or the failure of jails and hospitals to universally implement the screening elements of a successful elimination plan.
With the Biden Administration already struggling to get Congress to fund similar subscription plans for COVID-19 testing and treatment and flat out refusal from certain Senators to fund the Centers for Disease Control and Prevention’s sexually transmitted infections work despite data showing that under no uncertain terms the need exists, is there any real hope an appetite exists for similar funding to eliminate HCV in the United States?
One thing is clear, the cost of medication a payer sees (public or private) is not the biggest barrier to care for patients. Indeed, few patients care very much at all about what a payer’s costs are – patients care what their costs are and that includes costs not readily recognized by payers (like costs associated with time off work due to narrowed provider networks), or the time it takes providers to build trust in highly affected, highly marginalized communities. In fact, if policymakers wish to make the great investments necessary to eliminating HCV, they can start with sensible steps like requiring and enforcing hospitals to implement opt-out screening activities by way of rule making or legislation directing HCV screening to be a standard of care and integrated into the state’s essential health benefits benchmarks. Similarly, those same policymakers could require and enforce implementation of universal screening in all carceral settings or introduce legislation which requires departments of corrections to provide DAA to all incarcerated people diagnosed with HCV, regardless of cirrhosis status. States could require commercial health plans to cover DAAs at no cost sharing or require that all covered entities in that state charge a flat dispensing fee for DAAs (recognizing abusive dispensing fees for DAAs necessarily reduce the dollars available to support public health programming). States could dig into consolidation of access points to care to the exclusion of entire geographies hard hit by disparities.
There’s so much more to “access” to care than what a payer negotiates with a drug manufacturer and focusing exclusively on the issue of drug pricing. Without robust planning, reinvestment of “savings” into the logistical supports – including competitive wages and benefits packages for labor needs – necessary to feed the roots of this tree, all we’ll be left with is the low hanging fruit and rotten wood. And if we’re not careful, efforts at Ending the HIV Epidemic might end up looking much the same.
Navigating Monkeypox: Challenges Patients Face
The Community Access National Network (CANN) has launched an ambitious patient awareness campaign focused on the ongoing Monkeypox (MPV) outbreak. Its ‘MPV Response Project for People Living with HIV’ seeks to gather data and issue reports covering MPV in the United States. The reports will focus on epidemiological trends, vaccine access and equity, state-level access to vaccine and antiviral supplies, HIV and MPV co-infection risk and reporting, and the latest news related to the outbreak. The project is broad in scope, and it will tackle the MPV outbreak in a way that is both data-focused and patient-centric.
One of the first things CANN discovered while seeking this data is that, as is the case with many relatively new outbreaks, what data are available are both disjointed and confusing for any patients and affected communities to try to navigate. While the U.S. Centers for Disease Control & Prevention (CDC) has done an admirable job in creating a data reporting center that is relatively timely in terms of updates and data availability, their data are only as good as the data they receive from states.
This has been a problem across numerous disease states for decades: state epidemiology departments and state and local departments of health across the United States are almost universally chronically underfunded, understaffed, poorly regulated, and frequently disorganized and disconnected from even state-level, much less federal-level, networks and reporting standards.
The issues include:
1.) A lack of federal reporting standards and duplicative reporting across funding opportunities makes gathering, interpreting, and reporting data about disease states, such as MPV, an arduous and frustrating task.
An example, out of 55 reporting jurisdictions in the United States, MPV vaccine administration data presented by the CDC only accounts for 48 of them. The jurisdictions that are not included—Arizona, the District of Columbia, Indiana, Mississippi, Montana, Nebraska, and Puerto Rico—represent some of the poorest, most underserved patient populations in the U.S. Another example is that, of the 527,818 first-dose vaccine administrations reported in the U.S., an astounding 44,192 (8.4%) had no accompanying racial demographic information included.
This issue extends beyond vaccine reporting. Because MPV diagnoses and testing information reporting requirements are not standardized, each state can (and does) provide vastly different reporting based upon local standards. An example of this is that the state of Alabama breaks reporting of race categories into “White,” “Black,” and “Other.” This is despite the fact that 18.7% of Alabama’s population is Hispanic and 6% is Asian. Apparently, other races need not apply? Other states, such as Alaska, report their data directly to the CDC and provide no epidemiological information specific to the state on their state websites.
It can be incredibly frustrating, particularly as community service organizations and healthcare providers seek and use data as a tool for advocacy and patient engagement. It is certainly not a lofty expectation that each state’s governmental agencies be required to comport with some sort of standard. It is not a Herculean task for states to report data in a similar manner and format, but for this to become the standard, those at the federal law and policy needs to define and implement reporting requirements across disease states. As it stands, except in limited circumstances, states are not required to report these data, rather the CDC and other federal entities are left to negotiate data collection and sharing agreements as part of federal funding opportunities.
2.) States are still ill-prepared to deal with disease outbreaks.
One would think that, after nearly three years of dealing with a global pandemic outbreak, state departments of health might have figured out ways to deal with getting out information quickly, effectively, and in an organized manner. One would be wrong.
A big hurdle that CANN encountered while seeking state-level data was that state websites are, by and large, disorganized, confusing messes, even for the most experienced patient. For the average patient, trying to find information about MPV in most states requires several steps through difficult-to-find links to try to get where they need to go. Additionally, these pages are not uniformly located on state websites as opposed to state health department websites, when those websites are different, rather than integrated into the same website.
It is not too much to ask for state websites to have a featured link on the homepage of their websites for disease outbreaks that are of national and state-level importance? Indeed, many states and state health departments are quite familiar with using banner bulletins as seen during the initial crisis phase of the COVID-19 pandemic, as an example.
More galling is the fact that, despite nearly two years of administering mass vaccination drives, several states still don’t have this down to a science. An essential tool, only realized broadly on the federal level and through private partnerships, is a centralized vaccine scheduling system. Again, not to belabor the point, we did this with COVID-19 vaccines. We should be able to provide similar supports and patient access tools across all disease states and especially in infectious disease outbreaks in which a vaccine product is available.
Instead, what we have is a sort of secret club lottery that leaves patients with the onus of calling multiple healthcare providers and health departments just to check to see if the vaccine is available, and to try to schedule an appointment.
3.) Event-based testing and vaccination drives are effective, but underutilized and overly depended upon tools for addressing MPV.
There are two men for whom CANN has the absolute highest respect: Dr. Demetre Daskalakis and Dr. David Holland. Both of these men have taken amazing steps to go out into communities that are at high risk of transmission of diseases like HIV and MPV and deliver care where people are. From drag brunches to bathhouses to leather bars and circuit parties, they have consistently led the charge in a very public way. We have been doing this with HIV testing for decades but delivering point-of-care services at these locations has always been something of a taboo that needs to be overcome for reasons including addressing these outbreaks and overcoming social stigma which harms members of marginalized sexual and gender identity communities beyond these health disparities.
That said, it is a drop in the bucket. An important drop, but a drop, still. These events still run into issues of being accessible to people who work non-traditional hours, in service industries, do not have reliable transportation, or face any host of barriers, including social stigma which may make associating receiving care at these events unsafe or feel less welcoming for people outside of the immediately targeted community. Gay, bisexual, transgender, and other men who have sex with men, the population most affected by the current MPV outbreak, are not uniformly attracted to attending drag brunches or circuit parties but may lead full and active sex lives outside of those spaces. Considering the disparities already manifesting in the current MPV data, those people making up more and more of the share of new MPV diagnoses may well be best approached outside of these types of events. This is not to suggest we should cease having vaccination and testing events in sex positive spaces. This is to say our approach should be an “and” approach.
Beyond just COVID and MPV vaccines, we need to start delivering additional vaccine services in these locations, including influenza, Hepatitis A/B, Shingles, and the like.
4.) This nation needs round-the-clock medical services.
It’s time to leave behind the 8:00 – 4:00 and 9:00 – 5:00 physician and clinic hours of operation. We have known for decades that limited office hours force patients to choose between earning enough money to survive and receiving medical care. While some federally qualified health centers and STI clinics have offered services outside of traditional healthcare hours, many have not, insisting either their communities don’t need these extended hours or stating plainly, the funding does not exist to maintain the necessary staff to operate outside of traditional business hours. Even fewer private providers and health department clinics offer non-traditional hours.
It has never made sense that physicians' offices are only open during working hours…when people are expected to be working. Maybe it has to do with the idea that, at one point in American history, at least one parent was a stay-at-home parent who had the time and wherewithal to take kids and partners to the doctor’s office. Now that virtually every family member is required to work to make ends meet, we need a different solution.
The arguments against it consistently have to do with money—it’s expensive, and you can’t turn a profit. Healthcare provision should never be about making a profit at the expense of helping people. If that means that you find physicians, physician assistants, nurses, and administrative staff to work later shifts, that’s what it means. More likely, however, it means we need to address public and private payer efforts to constantly reduce provider reimbursement, given full credentialling to nurse practitioners in all states, and more readily hire non-clinical support staff from the communities immediately served by these entities.
Beyond the fact that this move would make basic healthcare services, such as testing and vaccination, more easily accessible to people who work during the day, it might also open up additional opportunities for more people to schedule appointments that don’t require sitting in a waiting room for a half-hour beyond their appointment time.
Editor’s Note: These issues may sound minor—like the sour grapes of an exhausted and annoyed patient advocate—but the truth is that patients get frustrated with the lack of user-friendliness of every aspect of our public health infrastructure.
Patients need to be able to find what they’re looking for without having to jump through seven different hoops to find out where to schedule a vaccine appointment. Patients should be able to find what they’re looking for without having to jump through seven different hoops and spend hours trying to find out where to schedule a vaccine appointment.
We should expect to be able to see if various locations actually have vaccine stock on hand without having to call an office and annoy an administrative employee to find out if they have it in stock and if any appointments are available.
It’s 2022, basic technology has existed since the mid-2000s and these better practices in public health and healthcare engagement have been known since the late 1980’s. It’s time to get it together.
Despite All Evidence in Support of Harm Reduction, Stigma Drives Public Attitudes
Earlier this year, a false claim spurred outrage from commentators and politicians regarding federal grant dollars for harm reduction programs across the country. Shortly after, in April 2022, the U.S. Department of Justice (DOJ) issued guidance on how the Americans with Disability Act (ADA) provides protections for people with opioid use disorder (OUD), which may also apply broadly to people with substance use disorder (SUD). From local and national advocates to actions from the Biden Administration, as a nation, the United States is facing the greatest change in drug policy since the Nixon Administration introduced a national policy officer (“drug czar”) on the issue. Forty years after Nancy Reagan’s “Just say no” campaign and the abject failure of the D.A.R.E. (drug abuse resistance education) program, the United States’ “War on Drugs” has only succeeded in criminalizing a health status with, up until relatively recent history, with broad bipartisan support. The effort to combat the stigma sewn into the fabric of our social attitudes towards drug use and misuse is coming to a fever pitch.
Scrolling through my own social media, I can across Representative Malinda Brumfield White’s post regarding a methadone clinic opening in Bogalusa – expressing “concern” for the location. The comments were rife with assumptions as to what the clinic might “mean” for the area and opposition to its location. The animus voiced is the exact type of animus an industrious litigator might cite to prove the attitudes DOJ cited as discriminatory and might spur actions which could violate the ADA. This clinic didn’t pop up out of nowhere, Louisiana’s legislature ordered a needs assessment on the impacts of the opioid crisis in 2018 after the Governor Bobby Jindal ushered in closing of most of the clinics in the state. Subsequently, the state’s health department identified a need to establish at least 10 new harm reduction service providers, focusing on addiction treatment centers (specifically, medication assisted treatment). A request for proposals (RFP) was issued in late 2021 and signed with Behavioral Health Group (BHG) shortly thereafter. But it’s just now that the local electeds are making noise about the clinic – as the operation is getting set to open.
Meanwhile, in California, Governor Gavin Newsom is rumored to be thinking about vetoing SB57, a piece of well-supported state legislation that would allow for pilot project locations for safe consumption sites. The project would be the largest yet seen, after New York allowed for a similar project last year, and is facing tough opposition even after the bill passed out of the state’s legislature, with a concerted campaign urging Governor Newsome to veto the bill. New York expanded their project this year thanks in large part due to the success of reversing hundreds of overdoses already.
Vermont’s Governor has already vetoed a similar bill. Though, that veto also axed additional funding for multiple modalities of harm reduction, including ones already existing in Vermont, Governor Phil Scott specifically cited the safe consumption sites projects as “counterintuitive” – a statement rooted in stigma (his assertation that data did not exist to support the project is false – see previous links on New York’s success). A bill in Kentucky to initiate a pilot project didn’t even get a committee hearing this year. And Rhode Island is finally finding a way to fund safe consumption sites – by using the state’s opioid settlement dollars. Rhode Island had already passed a law allowing study of safe consumptions sites, the legislation just did not include any funding to do so and those entities interested in opening sites were hard strapped to find enough private funding to open.
In other states, advocates are playing slower “games”, taking time to further educate their legislatures and communities. In North Carolina, experts took time to both debunk the claim the Biden Administration was pushing on smoking pipes but also how those same tools would be an improvement in harm reduction offerings already existing in the state. In Massachusetts, elected representatives are supportive of safe consumption sites but elected law enforcement isn’t. Those same elected law enforcement officials are peddling stigmatizing ideas with ominous sound bites like “let’s ask people in neighborhoods where they already exist and see if they feel it’s safer.” When there’s no one there to challenge these ideas, or journalists’ follow up questions aren’t answered, the dark clouds gather around pious suburbanites as if their own families aren’t one or two degrees of separation from experiencing the damaging impacts of an unabated overdose crisis.
Decades old attitudes which moralize a health condition as a personal failing and threat to our families hasn’t worked. Indeed, overdose deaths and non-fatal morbidities are on the rise…again. Despite having the tools, decades of behavioral intervention study, and a desperate need to address this issue, we keep seeing the same approached used over and over again – stigmatize, criminalize, and isolate. Our elected officials have an obligation to both educate themselves and advocate for more effective policy. The families affected by the opioid crisis, substance use disorder, Hepatitis C, and HIV are the voters and constituents these representatives are tasked to…represent. As advocates trudge on in sharing stories, we must leverage what we know to be true. This is indeed a moral fight – it is immoral and unethical to allow people to die with a callousness of disinterest, even triumph as if those deaths are somehow “deserved”. While our lawmakers are returning home as the federal legislative session comes to a brief break, they must also take this moment to lead their constituents in making the moral choice and support comprehensive harm reduction policies and programs.
Improvements to Public Health Guidelines, Despite Covid-19
2022 is off to a roaring Covid-19 start with both mainstream news and scientific outlets focusing on variant development, diversifying vaccines, and the impacts of the pandemic on various aspects of our lives. Last year, Community Access National Network opened our blog with discussing Covid-19’s Impact on HIV, HCV, and Substance Use Disorder and the theme crawled through our public policy discussions of the last year. While the topic is likely to set the frame for all variety of public health and policy throughout 2022, there is a necessity to discuss the developments in our space in spite of the distractions COVID has to offer.
Early 2021 found the Biden administration rescinding the “axe” the previous administration gave to the so-called “X” waiver, a requirement for providers to seek specified training in order to administer buprenorphine based medication assisted treatment for patients experiencing opioid use disorder. While providers and advocates hailed eliminating the X-waiver as a move toward advancing care, reports stated administration officials found problems with the rule as written, calling it “premature”. The Department of Health and Human Services (HHS) would later update treatment guidelines by way of formal notice posted to the federal register on April 28th, expanding eligibility of providers to administer the treatment when they “intend” to treat fewer than 30 patients a year. What enforcement looks like around the word “intent will be an area to watch as this area of public policy develops.
Later in the year, the Centers for Disease Control and Prevention (CDC) updated their Sexually Transmitted Infections Treatment Guidelines, the first overhaul since 2015. While the most significant updates to the guidelines are focused on the treatment of gonorrhea, an area of focus given the bacteria’s penchant for developing resistance to treatment, other highlights include aligning the guidelines with the CDCs 2020 recommendation for universal Hepatitis C screenings and adoption of the Advisory Committee on Immunization Practices (ACIP) recommendation for Human Papilloma Virus (HPV) “catch-up” vaccination schedules for people assigned male at birth. These and other additional updates were made, in part, because the CDC’s 2021 annual report found the United States facing the 6th consecutive year of STI increases.
Among ACIP’s many accomplishments in a year that found the panel meeting nearly twice as often as usual, a November meeting overshadowed by the endorsement of recommending Covid-19 vaccines for 5-11 year olds provided also found ACIP recommending universal adult Hepatitis B vaccination.
In a similar vein to the aforementioned updates (and with much rejoicing from advocates), the White House Office of National AIDS Policy “turned the lights back on” with the appointment of Harold Phillips as Director. Mr. Phillips provided an update to the National HIV/AIDS Strategy, announced in December with a focus on acknowledging structural barriers to achieving goals, including racism, stigma, and violence against transgender women. The plan, however, does not specifically outline ways to address these particularly challenging, systemic issues. President Biden also recognized World AIDS Day with a characteristically frank review of the history this country has with HIV and AIDS and the obstacles we still face in working to Ending the HIV Epidemic.
One of the last developments of 2021 included the CDC updating its clinical practice guidelines for pre-exposure prophylaxis for the prevention of HIV (PrEP). The update shifts language in such a way to encourage providers to more openly bring up the issue of PrEP with all patients rather than solely seeking to target “high-risk” populations. This move falls in-line with the efforts to reduce PrEP stigma among the broader public and, specifically, among providers. This was a particularly exciting development in light of the Food and Drug Administration’s (FDA) approval of cabotegravir (branded as Apretude) for PrEP. The long-acting injectable was first approved for the treatment of HIV in early 2021 and poses an extraordinary advancement in the potential for medication delivery mechanisms, improving adherence, and, ultimately, advancing efforts to End the Epidemic. Of note, pharmacy benefit managers, specifically CVS, anticipated this move as much as advocates and patients have. Despite a supposed commitment to investing in health equity with regard to HIV, CVS’ own “payor solutions” site boasts of the methods the entity will use seeking to delay or deny access to this and other innovative care under the need to “balance cost” with effective or curative treatments.
Looking into the new year, HHS’ annual policy report indicates the agency will seek to strengthen protections afforded to LGBTQ patients and more appropriately define discrimination in plan design, affecting patients living with HIV and HCV.
While these changes in direction and advancements in treatment are quite thrilling, advocates should be prepared to compete for space to be heard and anticipate familiar “foes” continuing to refuse to engage or finding ways to blockade access to care. Be they based in political ideal or industry priority or even from providers, patients and advocates would be better served when those who have traditionally disfavored advancing equity and access engaged in discussions on how to find the win-win for all parties. Community Access National Network remains committed to engaging stakeholders across interests in this space and looks forward to the good-faith efforts of those who seek to move these adversarial relationships to partnerships and even friendships.
HIV & Covid-19: A Story of Concurrent Pandemics
On September 20th, Johns Hopkins’ COVID data tracker totaled the “confirmed” (note: not “official”) number of deaths from COVID-19 in the United States to surpass 675,000 – or the estimated number of deaths in the US due to the 1918-1919 H1N1 influenza pandemic (colloquially called the “Spanish flu” because Spanish media were more willing to discuss the pandemic than most other countries). Forbes, STAT, and other large news outlets ran headlines like “Covid-19 overtakes 1918 Spanish flu as deadliest disease in American history” or included statements in their articles like “It was the most deadly pandemic in U.S. history until Monday, when confirmed coronavirus deaths overtook the death toll for the Spanish Flu.”
Which, as Peter Staley pointed out, isn’t factually accurate.
Image: Twitter.com - @peterstaley (Sep 20, 2021) “Um, HIV/AIDS? 700,000 U.S. deaths (and counting), according to the http://HIV.gov https://hiv.gov/federal-response/ending-the-hiv-epidemic/overview”
Staley would quickly admit COVID-19 would or already has likely overcome the death toll of HIV in the United States. While I agree with this analysis, I would add “for now”.
The very nature of HIV has made finding a “cure” or vaccine for the virus an oft sought after “holy grail” in pharmaceutical development. While that grail may have been snatched away by the attention COVID-19 is justly generating, this isn’t the first concurrent pandemic HIV has run alongside. The Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) both refer to the H1N1 influenza outbreak of the 2009-2010 flue season a “pandemic”. The problem of course isn’t just how deadly COVID-19 is, its’ how botched the domestic and global responses have been to the disease.
Viruses, after all, are opportunistic. They have a singular purpose: reproduce. As such, viruses thrive in environments – ecosystems, if you will – that are sorely neglected, lack coordinated responses, and are largely inequitable. But we knew that. We’ve known that with regard to global and domestic health disparities data for decades. As with personal health, emerging, urgent issues in public health reduce our capacity to address existing issues effectively.
As I mentioned in previous blogs, and has been recently noted by the Global Fund, COVID-19 has drastically reduced the efficacy of existing HIV, HCV, STI, and SUD programs. Even still, Global Fund’s report proves a rather interesting point – when meeting the demands of advocates for programs to provide patients with multi-month supplies of medications, meeting people in their own neighborhoods rather than in clinics, and providing at-home testing kits, communities can be activated in care at an exceptional level. Despite the COVID-19 pandemic raging, the needs of the HIV pandemic didn’t stop. And while meeting those needs faltered some (with 4.5% fewer mothers receiving vertical transmission prevention medications, an 11% drop in prevention programming, and a 22% reduction in testing services), in some areas meeting those needs thrived. Global Fund’s report found South Africa was able to increase the number of people receiving antiretroviral therapies by more than three times the baseline, even while fighting on two fronts.
Dr. Sioban Crowley, Head of HIV at the Global Fund, pointed out these program designs are not exclusive to HIV, “If we can keep 21.9 million people on treatment, we can probably deliver them a COVID test and a vaccine.”
Indeed, with the United States’ (and the world’s) response relying heavily on expertise gained in the fight against HIV, one can reasonably ask “If we know how to beat this, why aren’t we…just doing that?”
“That” being what advocates have long asked for: a more dedicated, equitable landscape and adequate support of our public health systems. As with COVID-19, a vaccine won’t “cure” us of HIV if the rest of the world cannot access it. As with HIV, if preventative services, adequate testing, and necessary education are not readily made available to people where they are, we will continue to fail in both fights. If we don’t wish to repeat the losses we’ve already experienced in the fight against HIV, then we cannot keep making the same mistakes of kicking the costs of these investments down the road and maybe, eventually “getting to it”.
As has been said many times through the latest pandemic, “the best time to do the right thing was yesterday. The next best time to do the right thing is today.” It’s time for us to do the right thing and stop allowing backbone public health programs to fall by the wayside in the face of the next emergency. Today, for the next few years, it’s COVID. We don’t need to “wait” for that to end. There’s two pandemics occurring, it’s time we act like it.
Biden Administration’s Healthcare Future is One of Promise & Peril
Last month, the Biden Administration issued a press release outlining a look toward the future of American health care policy. Priorities in the presser include ever elusive efforts around prescription drug pricing and items with steep price tags like expanding Medicare coverage to include dental, hearing, and vision benefits, a federal Medicaid look-alike program to fill the coverage gaps in non-expansion states, and extending Affordable Care Act (ACA) subsidies enhancements instituted under the American Rescue Plan (ARP) in March. Many of these efforts are tied to the upcoming $3.5 trillion reconciliation package.
President Biden renewed his call in support of the Democrats effort to negotiate Medicare prescription drug costs, enshrined in H.R. 3. Drug pricing reform has been an exceptional challenge despite relatively popular support among the voting public, in particular among seniors. The pharmseutical industry has long touted drug prices set by manufacturers do not represent the largest barriers to care and mandating lower drug costs would harm innovation and development of new products. Indeed, for most Americans, some form of insurance payer, public or private, is the arbiter of end-user costs by way of cost-sharing (co-pays and co-insurance payments). To even get to that point, consumers need to be able to afford monthly premiums which can range from no-cost to the enrollee to hundreds of dollars for those without access to Medicaid or federal subsidies. The argument from the drug-making industry giants is for Congress to focus efforts that more directly impact consumers’ own costs, not health care industry’s costs. Pharmaceutical manufacturers further argue mandated price negotiation proposals would harm the industry’s ability to invest the development of new products. To this end, the Congressional Budget Office (CBO) recently released a report giving some credence to this claim. The CBO’s report found immediate drug development would hardly be impacted as those medications currently “in the pipeline” would largely be safe, but a near 10% reduction in new drugs over the next 30 years. While new drug development has largely been focused on “personalized” medicine – or more specific treatments for things like cancer – implementing mRNA technology into vaccines is indeed a matter of innovation (having moved from theoretical to shots-in-arms less than a year ago). With a pandemic still bearing down on the globe, linking the need between development and combating future public health threats should be anticipated.
The administration’s effort to leverage Medicare isn’t limited to drug pricing. Another tectonic plate-sized move would seek to expand “basic” Medicare to include dental, hearing, and vision coverage. Congressional Democrats, while generally open to the idea, are already struggling with timing of such an expansion, angering Senator Bernie Sanders (I-VT) by suggesting a delay until 2028. While any patient with any ailments related to their oral health, hearing, and vision will readily tell you these are critical and necessary coverages, even some of the most common of needs, the private health care insurance industry generally requires adult consumers to get these benefits as add-ons and the annual benefit cap is dangerously low (with dental coverage rarely offering more than $500 in benefit and vision coverage capping at one set of frames, both with networks so narrow as to be near meaningless for patients with transportation challenges). While the ACA expanded a mandatory coverage for children to include dental and vision benefits in-line with private adult coverage caps, the legislation did nothing to mandate similar coverages for adults and did not require private payers to make access to these types of care more meaningful (expanded networks and larger program benefits to more accurately match costs of respective care).
The other two massive proposals the Biden Administration is seeking support for, more directly impact American health care consumers than any other effort from the administration: maintaining expanded marketplace subsidies and a federal look-a-like for people living in the 12 states that have not yet expanded Medicaid under the ACA’s Medicaid expansion provisions. The administration has decent data to back this idea, as the Centers for Disease Control and Prevention released a report showing a drop in the uninsured rate from 2019 to 2020 by 1.9 million people, largely attributed by pandemic-oriented programs requiring states to maintain their Medicaid rolls. The administration and Congressional Democrats are expected to argue subsequently passed legislation allowing for expanded subsidies and maintained Medicaid rolls improved access to and affordability of care for vulnerable Americans during the pandemic. As the nation rides through another surge of illness, hospitalizations, and death from the same pandemic “now isn’t the time to stop”, or some argument along those lines, will likely be the rhetoric driving these initiatives.
Speaking of the pandemic, President Biden outlined his administration’s next steps in combating COVID-19 on Thursday, September 9th. The six-pronged approach, entitled “Path out of the Pandemic”, includes leveraging funding to support mitigation measures in schools (including back-filling salaries for those affected by anti-mask mandates and improving urging the Food and Drug Administration [FDA] to authorize vaccines for children under the age of 12), directing the Occupational Safety and Health Administration (OSHA) to issue a rule mandating vaccines or routinized testing for employers with more than 100 employees (affecting about 80 million employees) and mandating federally funded health care provider entities to require vaccination of all staff, pushing for booster shots despite the World Health Organization’s call for a moratorium until greater global equity in access can be attained, supporting small businesses through previously used loan schemes, and an effort to expand qualified health care personnel to distribute COVID-19 related care amid a surge threatening the nation’s hospitals ability to provide even basic care. Notably missing from this proposal are infrastructure supports for schools to improve ventilation, individual financial support (extension of pandemic unemployment programs or another round of direct stimulus payments), longer-term disability systems to support “long-COVID” patients and any yet-unknown post-viral syndromes, and housing support – which is desperately needed as the administration’s eviction moratorium has fallen victim to ideological legal fights, states having been slow to distribute rental assistance funds, and landlords are reportedly refusing rental assistance dollars in favor of eviction. While the plan outlines specific “economic recovery”, a great deal is left to be desired to ensure families and individuals succeed in the ongoing pandemic. Focusing on business success has thus far proven a limited benefit to families and more needs to be done to directly benefit patients and families navigating an uncertain future.
President Biden did not address global vaccine equity in his speech, later saying a plan would come “later”. The problem, of course, is in a viral pandemic, variant development has furthered risks to wealthy countries with robust vaccine access and threatened the economic future of the globe.
To top off all of this policy-making news, Judge Reed O’Connor is taking another swing at dismantling some of the most popular provisions of the ACA. Well, rather, yet another plaintiff has come to the sympathetic judge’s court in an effort to gut the legislation’s preventative care provisions by both “morality” and “process” arguments in Kelley v. Becerra. The suit takes exception to a requirement that insurers must cover particular preventative care as prescribed by three entities within the government (the Health Resources Services Administration – HRSA, the Advisory Committee on Immunization Practices – ACIP, and the Preventative Services Takes Force – PSTF), which require coverage of contraceptives and pre-exposure prophylaxis (PrEP) with no-cost sharing to the patient, among a myriad of other things – including certain vaccine coverage. By now, between O’Connor’s rabid disregard for the rights of lesbian, gay, bisexual, and transgender Americans and obsessive effort to dismantle the ACA at every chance he can – both to his own humiliation after the Supreme Court finally go their hands on his rulings – Reed O’Connor may finally have his moment to claim a victory – I mean – the plaintiffs in Kelley may well succeed due to the Supreme Court’s most recent makeover.
As elected officials are gearing up for their midterm campaigns, how these next few months play out will be pretty critical in setting the frame for public policy “successes” and “failures”. Journalists would do well to tap into the expertise of patient advocates in contextualizing the real-world application of these policies, both during and after budget-making lights the path to our future – for better or worse.
Amid HIV Outbreaks, Covid-19 Fractures Existing Public Health Efforts
“Every health disparity map in the United States is the same,” Alex Vance, Senior Director of Advocacy and Public Policy at the International Association of Providers in AIDS Care, has repeatedly stated when discussing the COVID-19 pandemic and the very real risks of “back sliding” in our moderate advancements in the United States’ effort to End the HIV Epidemic. There’s no better way to demonstrate this than by showing you.
As another “wave” of Covid-19 ravages the country, increasing cases, hospitalization rates, and eventually deaths, existing public health needs around HIV, viral hepatitis, and sexually transmitted infections continue to be strained, pushed to the back burner and most often in geographic areas where we need to be able to juggle more, not less; particularly across the South. Unlike Covid-19 outbreaks, which receive fairly immediate attention in terms of reporting and response, HIV outbreaks can and do often take a year or more to notice and begin action to address. While there’s concern about juggling the demands of addressing concurrent pandemics, some (certainly not all) of this reporting and response is beginning to speed up with regard to HIV.
West Virginia’s Kanawha County HIV outbreak is considered a 2020 outbreak, though just recently received a report from the Center’s for Disease Control & Prevention (CDC) on next steps and recommendations to address. Despite these recommendations including supporting syringe exchange programs and community-based services, local officials continue a politically oriented response by seeking to limit the support of syringe exchange programs, threatening their ability to operate and aid in addressing the needs of the local community. Another outbreak in Michigan’s Upper Peninsula was identified in July of this year, with rural Kalkaska County reporting a higher rate of new HIV diagnoses than even Detroit. Kalkaska County is so similarly situated to Scott County, Indiana, it’s striking. Louisville, Kentucky has reported almost as many new HIV diagnoses in the first half of 2021 as the area does annually. And Duluth, outside of Saint Louis, Minnesota, joined neighboring Hennepin and Ramsey Counties with declared outbreaks tied to 2019 and 2018, respectively.
What’s important to note about 2020’s marked reduction in HIV screenings is not just the delay in newly diagnosing people living with HIV, but the lack of ability to link people to care upon diagnosis, beginning antiretroviral therapy and taking steps to reduce the person’s viral load. With at-home testing being the substitute offering, linkage to care and counseling for people self-testing may be hampered according to some concerned advocates. Achieving viral suppression also reduces the possibility of transmitting HIV by way of sexual contact to zero (“Undetectable = Untransmittable”) – creating a process where people living with HIV are not just a patient group needing identification, but play a critical role in preventing new transmissions.
In reviewing the possibilities of delayed care and delayed screening, public health officials and advocates should remember a new diagnosis is not necessarily indicative of a new transmission. A potential problem in and of itself, in assessing Covid-19 disruptions in screening and care, is the possibility of a “bottle neck” of new testing revealing new HIV diagnoses which otherwise might have been identified in the previous year if not for stay-at-home orders, education and public awareness campaigns, and community health care providers having had to take a step or shift gears entirely from HIV to Covid-19. It will take years for us to truly understand the breadth and reach of Covid-19 on the world’s only concurrent pandemic, even in the “most advanced country in the world”.
What can already be well-appreciated and should be well-understood is we cannot afford to keep asking community-based health care providers and community partners in combatting the domestic HIV epidemic to keep sacrificing HIV screening and linkage to care in order to address Covid-19. What must be prioritized is funding, programming, training, and most importantly hiring of new talent in addition to existing programs in order to address both sets of needs.
As I summarized in a previous blog, capacity has been breached, we cannot afford to keep asking public health to do more with less and expect to succeed in addressing Covid-19, HIV, viral hepatitis, STIs, or the opioid epidemic.